Arterial aneurysms are commonly encountered in adult clinical practice, arising from multifactorial vascular degeneration and typically presenting between the sixth and eighth decades of life. Comparatively rare entities, venous aneurysms frequently result from congenital deficiencies of the vessel wall rather than degenerative processes, and more often come to attention in the pediatric population.1–3 When encountered in children, neck masses can pose a diagnostic dilemma due to the relatively broad differential diagnosis in this age group. However, the differential diagnosis is limited when a neck mass enlarges when performing a Valsalva maneuver. Diagnostic considerations for a neck mass that enlarges with Valsalva maneuver include superior mediastinal tumor or cyst, laryngocele, or jugular phlebectasia.4
Duplex ultrasonography scanning is usually sufficient for the diagnosis of a venous aneurysm, but three-dimensional ultrasonography, computed tomography, magnetic resonance imaging with magnetic resonance angiography/magnetic resonance venography, and catheter-directed venography can also be performed to improve morphologic evaluation.5

Figure 1: Right lateral view of the patient without (right) and with the Valsalva maneuver (left).
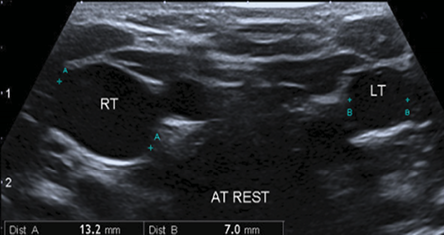
Figure 2: Grayscale ultrasound of internal jugular veins on both sides at rest showing the clear difference in the diameter of both veins with relative dilatation of the right side reaching 13 mm.
Case report
A four-year-old boy with no known medical illnesses presented to our clinic with a right-sided painless neck swelling he had since the age of two. The swelling was evident only while straining and crying and disappeared at rest. The boy had no history of pain, fever, facial puffiness, change in the voice, and no difficulty in breathing or swallowing. The family gave no history of neck trauma or previous neck infection.
On physical examination, he looked healthy. Neck examination did not reveal any obvious mass. A 3 × 3 cm mass appeared on the right side of his neck on straining and while performing the Valsalva maneuver, the mass appeared from below the right sternocleidomastoid muscle and extending up to the right anterior triangle of the neck [Figure 1]. On palpation, the swelling felt cystic, non-tender, soft, non-mobile, and the overlying skin was normal. No bruit or pulsation was noted over the swelling, and it did not transilluminate with light. Ear, nose, and throat examinations were unremarkable. A small right testicular hydrocele was diagnosed by the surgical team and conservative treatment was planned. Neck ultrasound was performed and revealed significant dilatation of the right internal jugular vein (reaching up to 31 mm in diameter) during the Valsalva maneuver[Figure 2 and 3].
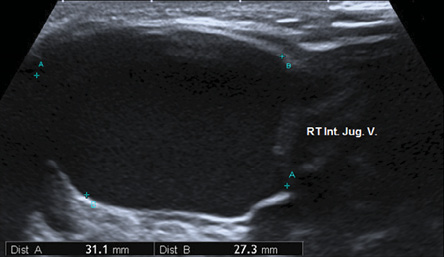
Figure 3: Grayscale ultrasound shows localized dilated right internal jugular vein, which increased during the Valsalva maneuver reaching its maximum luminal diameter of about 31 mm.
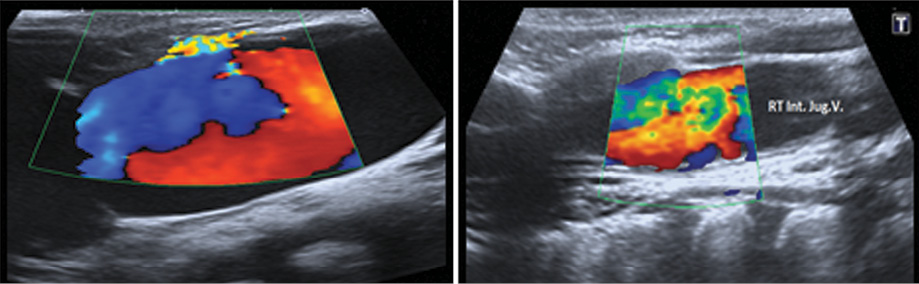
Figure 4: Color Doppler imaging study of the same vein showing turbulence of the blood flow at the site of ectasia with the absence of any filling defect (no thrombosis).
Doppler study showed color aliasing, which indicate ectasia of the venous wall [Figure 4]. Since the swelling was asymptomatic, the parents were counseled and the patient was kept under regular follow-up.
Discussion
Jugular vein phlebectasia (JVP), also known as a venous congenital cyst, venous aneurysm, venous ectasia, or essential venous dilatation, refers to a congenital fusiform dilatation of the jugular vein. It appears as a soft, compressible mass in the neck during straining, coughing, crying, and sneezing and is triggered by the Valsalva maneuver.6 Internal jugular ectasia was first described by Zukschwerdt and subsequently characterized by Gerwgi.7 Possible causes of JVP are gross anatomic abnormality, mechanical compression or neck trauma, congenital structural defects, and idiopathic causes.6 JVP is mostly seen in children and occurs in males twice as often than females. JVP usually presents on the right side. La Monte et al,8 hypothesized that ectasia is more common on the right side because the right innominate vein lies in contact with the right apical pleura. Hence, any increase in intrathoracic pressure could be directly communicated to the right internal jugular vein. The left vein was not subject to this stress as it is placed more medially. Anatomical factors that predispose to increased pressure in the right brachiocephalic vein compared to the left and in turn to a higher incidence of ectasia of the right internal jugular vein include the right brachiocephalic vein travelling in the same direction of superior vena cava; the diameter of the right brachiocephalic vein being greater than the left; right brachiocephalic vein being shorter than the left; and valves present in the left brachiocephalic vein (occurs in 4–8%).
JVP is a benign condition and is usually asymptomatic.9 JVP should be differentiated from cystic neck swelling as laryngocele, branchial cyst, cystic hygroma, cavernous hemangioma, superior mediastinal mass, and hypertrophy of pulmonary apex.9 Absence of a wide mediastinum or air in the mass on simple chest films eliminates mediastinal tumor or laryngocele respectively. Ultrasonography combined with Doppler flow imaging is diagnostic and shows color aliasing, as seen in our case.
Asymptomatic JVP does not need any intervention and must be followed-up conservatively. Our patient is currently being followed-up and asymptomatic. Surgical options are usually indicated for esthetic purposes or presence of complications.10 In most reported cases, the internal jugular vein and associated veins have been ligated, with the loss of the normal venous drainage pattern on that side. Other interventions described include longitudinal constriction suture venoplasty and partial resection of the phlebectasia.11 Both options have been reported to be safe and successful in eliminating phlebectasia. Postoperative complications commonly reported are thrombosis and Horner’s syndrome.12 Balik et al,13 reported a case of jugular phlebectasia with thrombosis and suggested surgical removal of the involved segment without delay because of the thrombosis. Our case had no such complications. Upon searching the English literature, published between 1996 and 2001, 31 cases of internal jugular phlebectasia in children were described in the UK mostly occurring on the right side.14 More than 100 cases of phlebectasia involving the neck veins including anterior and external jugular veins have been reported in the world literature, but there were no reported cases or syndromes that associate JVP with hydrocele as in our case. Both JVP and hydrocele are congenital.
A hydrocele is a collection of serous fluid that results from a defect or irritation in the tunica vaginalis of the scrotum. Hydroceles also may arise in the spermatic cord or the canal of Nuck. A communicating hydrocele is similar to a hernia except that the sac connecting the abdomen to the scrotum contains only fluid rather than abdominal contents. A noncommunicating hydrocele is a collection of scrotal fluid isolated from the abdomen. Noncommunicating hydroceles are the most common type of hydrocele globally, affecting more than 30 million men and boys. As the pathophysiology of both JVP and hydrocele are different, the concurrent occurrence of JVP and hydrocele, as seen in our case, is probably incidental.
Conclusion
Congenital internal jugular phlebectasia is a rare entity. The diagnosis should be considered whenever a child presents with a neck mass and enlarged by maneuvers increasing intrathoracic pressure (such as the Valsalva maneuver). The diagnosis must be confirmed by imaging. Surgery is only indicated in the presence of complications. Although right internal JVP has been reported many times, it is still an interesting condition, which could be easily missed.
Disclosure
The authors declared no conflicts of interest.
references
- Calligaro KD, Ahmad S, Dandora R, Dougherty MJ, Savarese RP, Doerr KJ, et al. Venous aneurysms: surgical indications and review of the literature. Surgery 1995 Jan;117(1):1-6.
- 2. Sakallioğlu AE, Yağmurlu A, Yağmurlu B, Gökçora HI. An asymmetric ballooning of the neck: Jugular vein aneurysm. J Pediatr Surg 2002 Jan;37(1):111-113.
- 3. Fishman G, DeRowe A, Singhal V. Congenital internal and external jugular venous aneurysms in a child. Br J Plast Surg 2004 Mar;57(2):165-167.
- 4. Sander S, Eliçevik M, Unal M, Vural O. Jugular phlebectasia in children: is it rare or ignored? J Pediatr Surg 1999 Dec;34(12):1829-1832.
- 5. Gillespie DL, Villavicencio JL, Gallagher C, Chang A, Hamelink JK, Fiala LA, et al. Presentation and management of venous aneurysms. J Vasc Surg 1997 Nov;26(5):845-852.
- Sander S, Eliçevik M, Unal M, Vural O. Jugular phlebectasia in children: is it rare or ignored? J Pediatr Surg 1999 Dec;34(12):1829-1832.
- 2. Gerwig WH Jr. Internal jugular phlebectasia. Ann Surg 1952 Jan;135(1):130-133.
- 3. LaMonte SJ, Walker EA, Moran WB. Internal jugular phlebectasia. A clinicoroentgenographic diagnosis. Arch Otolaryngol 1976 Nov;102(11):706-708.
- 4. Abdulla AS, Aldabagh MH. Congenital phlebectasia of internal jugular vein. Dohuk Med J 2008;2(1):155-160.
- 5. Inci S, Bertan V, Kansu T, Cila A. Horner’s syndrome due to jugular venous ectasia. Childs Nerv Syst 1995 Sep;11(9):533-535.
- 6. Hu X, Li J, Hu T, Jiang X. Congenital jugular vein phlebectasia. Am J Otolaryngol 2005 May-Jun;26(3):172-174.
- 7. Kwok K-L, Lam H-S, Ng DK. Unilateral right-sided internal jugular phlebectasia in asthmatic children. J Paediatr Child Health 2000 Oct;36(5):517-519.
- 8. Balik E, Erdener A, Taneli C, Mevsim A, Sayan A, Yüce G. Jugular phlebectasia in children. Eur J Pediatr Surg 1993 Feb;3(1):46-47.
- 9. Paleri V, Gopalakrishnan S. Jugular phlebectasia: theory of pathogenesis and review of literature. Int J Pediatr Otorhinolaryngol 2001 Feb;57(2):155-159.