The Buthidae scorpion family is the largest and most common venomous species found in the Mediterranean and Arabian Peninsula and includes genera of Buthacus, Leiurus, Androctonus, and Vachoniolus.1,2 The Scorpiones scorpion family is also found in Oman.3 The annual incidence of scorpion stings globally is estimated to be 1.5 million.4 In Oman, scorpion stings account for 20% of human exposures due to animal bites and stings.5 There are also regional variations with only 6% of scorpion stings reported in Muscat.4 Temperature and humidity are important factors contributing to the summer seasonal variation of scorpion stings.1,6 Although rarely encountered, systemic complications from scorpion stings have been reported including, but limited to, disseminate intravascular coagulation, anaphylaxis, acute pancreatitis, encephalopathy, acute hepatic injury, pulmonary edema, acute renal failure, metabolic acidosis, and stroke.7 A long-lasting demyelinating polyneuropathy following a scorpion sting was reported at Sultan Qaboos University Hospital (SQUH) despite antivenom treatment.8 A prospective, randomized controlled study conducted in Tunisia including 600 patients with scorpion sting found no significant difference in hospital stay and occurrence of life-threatening complications (shock or pulmonary edema) between steroid and placebo treatment.9,10 Topical 5% lidocaine was found to be the most significantly effective modality in reducing pain after stings.11 There was no difference found in complications related to scorpion stings when using prazosin compared to other treatment modalities in a small study done in India.12 Antivenom use for scorpion stings reported in the literature is variable.
No difference has been found in the outcome or admission rate between patients receiving antivenom four hours post-sting compared for patients with similar clinical presentations receiving placebo.10,11 Another study published in 1999 showed no beneficial ‘resolution of symptoms’ of antivenom administration after four hours compared to supportive treatment.13 Although antivenom induced anaphylactic shock was reported only in 1.3%, motion sickness was reported in 57% of patients who received antivenom.9
Methods
Our study included two parts. The first was a retrospective observational study of cases presenting to the emergency department (ED) at SQUH after scorpion stings over a 17-month period from March 2016 to July 2017. Data were collected from an electronic medical record system (Trakcare) for all patients triaged with bites and stings. The study did not include the name of the scorpion family involved. Collected data included demographic data (age, gender, sex, month of sting), clinical characteristics (clinical symptoms, investigation), and management (medication, disposition).
Cases were included if a scorpion sting was confirmed by seeing the scorpion and cases were excluded if no scorpion sting occurred, if the bite or sting was from something other than a scorpion, or if it was an unknown sting.
The second part of our study was a survey conducted to evaluate physicians’ knowledge regarding the management of scorpion stings in EDs at two different tertiary hospitals in Muscat (SQUH and Royal Hospital) and a secondary hospital (Armed Forces Hospital).
The primary outcome measured was the management aspects of scorpion stings, and we also investigated the incidence of scorpion stings at SQUH during the study period.
We used standard statistical tests to analyze the comparative demographics of the groups for gender and age. Means and medians were calculated for continuous variables. Data were analyzed using Microsoft Excel™ (2010).
Results
The total number of scorpion stings seen at SQUH ED between March 2016 and July 2017 was 128. Table 1 represents the demographic characteristics of the patients. Most incidences of stings occurred during the summer from May to July (59.4%, n = 76) with the peak occurring in June. Over half of the patients (55.5%, n = 71) stayed in the ED for less than two hours, 39.1% (n = 50) stayed two to four hours, and only 5.5% (n = 7) stayed more than four hours.
Table 1: Demographic characteristics of patients stung by scorpions.
|
Age |
|
|
|
Adult patient |
108 |
84.4 |
|
Pediatric patient |
20 |
15.6 |
|
Sex |
|
|
|
Male |
96 |
75.0 |
Table 2 represents the clinical features of patients with scorpion stings. The majority of patients (97.7%, n = 125) had localized pain, swelling was seen in 14.8% (n = 19) of patients, and localized redness in 7.0% (n = 9) of patients. Seventeen patients had systemic symptoms, with tachycardia being the most common in 15 (11.7%) patients, followed by hypertension in four (3.1%) patients. Vomiting and chest pain were seen in one patient each.
Table 3 shows the investigations done. Whole blood bedside clotting test was done in 15 (11.7%) patients followed by a coagulation test in seven (5.5%) patients. An electrocardiogram was done only for four patients. Most patients (54.7%, n = 70) received local anesthesia, and the remaining (43.0%, n = 55) patients received tetanus toxoid [Figure 1].
Stung patients received oral analgesia (27.0%, n = 35) followed by intramuscular analgesia (23.4%, n = 30); only 2.3% (n = 3) received intravenous analgesia. No patients received scorpion antivenom. Patients were discharged on non-steroidal anti-inflammatory drugs (42.2%, n = 54) and paracetamol with or without codeine (20.3%, n = 26) [Table 4].
Table 2: Clinical features of patients with
scorpion stings.
|
Local signs |
|
|
|
Pain |
125 |
97.7 |
|
Swelling |
19 |
14.8 |
|
Redness |
9 |
7.0 |
|
Systematic symptoms |
|
|
|
Tachycardia |
15 |
11.7 |
|
Vomiting |
1 |
0.8 |
|
Chest pain |
1 |
0.8 |
The survey was collected from 89 physicians working in the ED; nine were excluded as they never managed a scorpion sting. Most respondents were junior doctors working (60.0%, n = 48) and managed both adult and pediatric cases (46.3%, n = 37).
Most physicians (98.8%, n = 79) treated patients with local symptoms (local pain and swelling). Only 13.8% (n = 11) treated patients with systemic symptoms. Analgesia were the main management prescribed (88.9%); 33.8% (n = 27) used intravenous analgesia, 21.3% (n = 17) used intramuscular analgesia, and 33.8% (n = 27) used oral analgesia. The other common modality of treatment was local anesthesia (81.3%, n = 65). Other less frequently used modalities of treatment were tetanus toxoid (32.5%, n = 26) and antihistamines (30.0%, n = 24). Only 3.8% (n = 3) used steroids, and 15.0% (n = 12) used antivenom.
When asked the question, “What is the most effective management of scorpion stings?” most physicians (80.0%, n = 64) chose local anesthesia while only 11.3% (n = 9) chose intravenous analgesia. Antivenom was thought to be the most effective management in 8.8% (n = 7) of physicians.
Table 3: Lab investigations in patients with scorpion stings, n (%).
|
Full blood count |
5 (3.9) |
123 (96.1) |
|
Coagulation |
7 (5.5) |
121 (94.5) |
|
Urea and electrolyte |
4 (3.1) |
124 (96.9) |
|
Liver function test |
2 (1.6) |
126 (98.4) |
Twenty percent (n = 16) of physicians had never used local anesthesia for the management of scorpion stings. Of these, 81.3% (n = 13) reasoned their choice for not using it as “due to pain control by IV analgesia.” The rest thought their patients had tolerable pain. Around 32.5% (n = 26) of physicians ordered whole blood bedside clotting test; 69.2% (n = 18) were junior doctors, and only 30.8% (n = 8) were senior emergency physicians [Figure 2]. The most common reason given for ordering by 84.6% (n = 22) of physicians was due to fear that scorpion stings cause coagulopathy.
Table 4: Discharged medication given to patients of scorpion stings.
|
Non-steroidal anti-inflammatory drugs |
54 (42.2) |
|
Paracetamol +/- codeine |
26 (20.3) |
|
Antihistamine |
7 (5.1) |
|
H2 blockers |
2 (1.6) |
|
Steroid |
1 (0.8) |
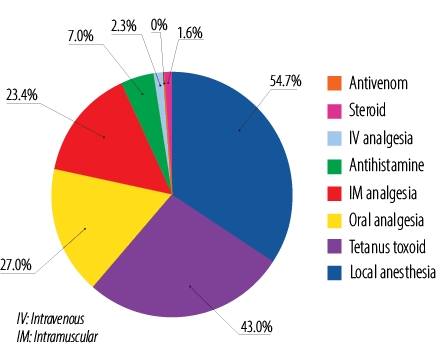
Figure 1: Treatment given to patients in the emergency department for the treatment of scorpion stings.

Figure 2: Correlates the use of whole blood bedside clotting test with the level of treating providers.
Discussion
Our study found that over half (54.7%) of patients stung by scorpions received local anesthesia in the ED, 27.3% received tetanus toxoid, and only 2.3% received intravenous analgesia. A regional randomized controlled study found that topical lidocaine was an effective and safe treatment for scorpion stings associated with pain in patients with no systemic signs and symptoms of envenomation.11 In the same study, some of the providers thought that oral and intravenous analgesia were better treatments than local anesthesia for pain management. The use of steroids in severe scorpion-envenomed patients was not found to improve their outcome.14 In our study, steroid was used only in 3.8% of patients.
Children represented around 15.6% of patients with scorpion stings in our study, but none of them developed serious envenomation or needed antivenom; although children are usually at greater risk of developing severe scorpion envenomation requiring administration of antivenom.15,16 Most patients in our study had local symptoms; the most common systematic manifestation was tachycardia. Scorpion venom is known to cause stimulation of neurotransmitters and catecholamines, which explain the tachycardia.17 All our patients who undergone blood investigation had normal results including coagulation profile.
The release of cytokines and inflammatory mediators induced by the venom have been implicated in hepatic and hematologic derangements, as well as direct action of scorpion venom on liver endothelial and blood cells.18,19 Whole blood bedside clotting test was done in 11.7% of patients and all had normal results. Certain species of scorpions can cause derangement in the bedside clotting test, such as the Venezuelan Tityus discrepans scorpion venom, which contains an anticoagulant component20 and is different from species available in Oman. A retrospective study of 290 patients in Iran reported that hemoglobinuria, coagulopathy, transfusion, and kidney problems were more commonly seen in patients admitted more than 24 hours after the sting.21 All our patients presented within a few hours. This study included only hospitals in Muscat governorate and might not necessarily represent other governorates in term of systemic toxicity and utilization of antivenom.
This study had several significant limitations. First, as for any retrospective study, there were missing information in some cases. Second, there was no patient follow-up, and some may have developed more symptoms after being discharged from our hospital and were seen in different hospitals. However, this is unlikely as they were given discharge instructions to come back if they developed any alarming signs, but none had a repeat visit. Our survey had the potential for recall bias, as some of the doctors may not have remembered their management of scorpion stings.
Conclusion
Most scorpion sting cases managed in our hospital had local symptoms. Tachycardia was the most common systemic manifestation seen. Local anesthesia infiltration is the recommended management for scorpion sting. Bedside clotting test was not commonly ordered and mainly requested by junior doctors. Analgesia was the main management followed by local anesthesia infiltration. Scorpion antivenom is rarely used.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Bawaskar HS, Bawaskar PH. Scorpion sting: update. J Assoc Physicians India 2012 Jan;60:46-55.
- 2. Al-Asmari AK, Al-Saif AA, Abdo NM. Morphological identification of scorpion species from Jazan and Al-Medina Al-Munawara regions, Saudi Arabia. J Venom Anim Toxins Incl Trop Dis 2007;13(4):821-843.
- 3. Lourenço WR, Huber D. Two new species of scorpions (Scorpiones, Buthidae) of the genus Paraorthochirus Lourenço & Vachon from Oman. Zool Middle East 2000 Jan;20(1):125-136.
- 4. Chippaux JP. Emerging options for the management of scorpion stings. Drug Des Devel Ther 2012;6:165-173.
- 5. Lall SB, Al-Wahaibi SS, Al-Riyami MM, Al-Kharusi K. Profile of acute poisoning cases presenting to health centres and hospitals in Oman. East Mediterr Health J 2003 Sep-Nov;9(5-6):944-954.
- 6. Alkahlout BH, Abid MM, Kasim MM, Haneef SM. Epidemiological review of scorpion stings in Qatar. The need for regional management guidelines in emergency departments. Saudi Med J 2015 Jul;36(7):851-855.
- 7. Gadwalkar SR, Bushan S, Pramod K, Gouda C, Kumar PM. Bilateral cerebellar infarction: a rare complication of scorpion sting. J Assoc Physicians India 2006 Jul;54:581-583.
- 8. Alsawafi FA, Alhinai H, Alhattali B, Awad S, Alreesi A, Alshamsi M. Demyelinating polyneuropathy following scorpion sting envenomation; a case report and review of literature. Asia Pac J Med Toxicol 2015;4(4):161-164.
- 9. Rodrigo C, Gnanathasan A. Management of scorpion envenoming: a systematic review and meta-analysis of controlled clinical trials. Syst Rev 2017 Apr;6(1):74.
- 10. Abroug F, Nouira S, Haguiga H, Elatrous S, Belghith M, Boujdaria R, et al. High-dose hydrocortisone hemisuccinate in scorpion envenomation. Ann Emerg Med 1997 Jul;30(1):23-27.
- 11. Aksel G, Güler S, Doğan NÖ, Çorbacioğlu ŞK. A randomized trial comparing intravenous paracetamol, topical lidocaine, and ice application for treatment of pain associated with scorpion stings. Hum Exp Toxicol 2015 Jun;34(6):662-667.
- 12. Gupta V. Prazosin: a pharmacological antidote for scorpion envenomation. J Trop Pediatr 2006 Apr;52(2):150-151.
- 13. Belghith M, Boussarsar M, Haguiga H, Besbes L, Elatrous S, Touzi N, et al. Efficacy of serotherapy in scorpion sting: a matched-pair study. J Toxicol Clin Toxicol 1999;37(1):51-57.
- 14. Bahloul M, Chaari A, Dammak H, Ben Algia N, Medhioub F, Ben Hamida C, et al. Impact of hydrocortisone hemisuccinate use on outcome of severe scorpion-envenomed adult patients. Am J Ther 2014 Nov-Dec;21(6):e181-e188.
- 15. Bosnak M, Levent Yilmaz H, Ece A, Yildizdas D, Yolbas I, Kocamaz H, et al. Severe scorpion envenomation in children: Management in pediatric intensive care unit. Hum Exp Toxicol 2009 Nov;28(11):721-728.
- 16. Dudin AA, Rambaud-Cousson A, Thalji A, Juabeh II, Abu-Libdeh B. Scorpion sting in children in the Jerusalem area: a review of 54 cases. Ann Trop Paediatr 1991;11(3):217-223.
- 17. Zayerzadeh E, Mirakabadi AZ, Koohi MK. Biochemical and histopathological study of Mesobuthuseupeus scorpion venom in the experimental rabbits. Arch Razi Inst 2011;66(2):133-138.
- 18. Cusinato DA, Souza AM, Vasconcelos F, Guimarães LF, Leite FP, Gregório ZM, et al. Assessment of biochemical and hematological parameters in rats injected with Tityus serrulatus scorpion venom. Toxicon 2010 Dec;56(8):1477-1486.
- 19. Heidarpour M, Ennaifer E, Ahari H, Srairi-Abid N, Borchani L, Khalili G, et al. Histopathological changes induced by Hemiscorpius lepturus scorpion venom in mice. Toxicon 2012 Mar;59(3):373-378.
- 20. Brazón J, Guerrero B, Arocha-Piñango CL, Sevcik C, D’Suze G. [Effect of Tityus discrepans scorpion venom on global coagulation test. Preliminary studies]. Invest Clin 2008 Mar;49(1):49-58.
- 21. Rahmani AH, Jalali AI. Symptom patterns in adult patients stung by scorpions with emphasis on coagulopathy and hemoglubinuria. J Venom Anim Toxins Incl Trop Dis 2012;18(4):427-431.