| |
Tear Film Status in Patients Attending the Eye Clinic in South Sharqiya Region
Belur R Keshav, Biju Mathews, Mary Joseph, George Zachariah, Thara Ideculla
ABSTRACT
Objective: To study the tear film profile of patients attending the eye clinic of Sur hospital of South Sharqiya region of Oman and to study the epidemiology of patients having abnormal tear film profile. Method: Patients attending the eye clinic of Sur hospital and B. Ali eye clinic were asked about the clinical symptoms relevant to dry eye and subjected to tear film tests namely TBUT (Tear Break up Time) and Schirmer’s 1 to assess tear film profile. Patients with irregular corneas were excluded from the study. Overall 127 patients were included in the study. Results: 42.5% (95% CI: 33.9% to 51.1%) of patients examined had abnormal tear film profile with patients >30 years 56.75% (95% CI: 45.4% to 68%) showing abnormality more often and females 40.3% (95% CI: 29.3% to 51.2%) outnumbered males. Burning was the main symptom in patients with abnormal tear film profile. Conclusion: We infer that a large number of patients had abnormal tear film profile most of them were asymptomatic and trachoma figured prominently amongst the diseases in cases with abnormal tear film profile.
Keywords: Dry eye, Tear Break up Time (TBUT), Schirmers.
Submitted: 9 July 2007
Reviewed: 29 July 2007
Accepted: 6 September 2007
From the Department of Ophthalmology, Sur Hospital & Bu Ali Hospital, South Sharqiya Region, Sultanate of Oman.
Address Correspondence and reprint requests to: Dr. Belur R Keshav, Department of Ophthalmology, Sur Hospital, South Sharqiya Region, Oman.
Email: keshavraj_2000@yahoo.com
INTRODUCTION
Dry eye is a very common and serious disorder, which is one of the most under diagnosed or wrongly diagnosed in ophthalmic set up. This leads to patients getting wrong medications for their problem which in turn aggravates the problem of dryness or fails to relieve him leading to the patient seeking help from another doctor who in turn dispenses another medicine thus setting up a vicious cycle. This may lead to patient getting frustrated and seek help from traditional doctors or quacks and this in turn may lead to serious eye threatening disorders like corneal ulcers , glaucoma etc., Dry eye was defined by the national eye institute in 1993 as a “disorder of the tear film due to tear deficiency or excessive evaporation which causes damage to the interpalpaebral ocular sauce and is associated with symptoms of discomfort”. The prevalence of blindness is still not precisely known. In epidemiological studies of dry eye performed in a variety of patient population the prevalence ranged from 6% of an Australian population 40 years and older,1 to 15% of a population over the age of 65 in Maryland USA.2 Most studies showed increased prevalence with age and in women. In Thailand the prevalence was found to be 34% (going by symptoms alone).3 Among Chinese the prevalence was found to be 33.7%.4 Amongst the causes of dry eye, Sjogrens syndrome amounted to 22% of the cases studied.5 Presently among the non sjogren causes, Laser-Assisted in situ Keratomileusis (LASIK) is one of the predominating causes.6 Trachoma is one of the important causes in areas which were endemic for trachoma as it cause conjunctival scarring and reduction of goblet cell density,7 which secretes the mucus layer of the tear film apart from its tendency to affect the meibomian secretions which effect the lipid layer of the tear film which is so important for prevention of tear evaporation.8 Thus trachoma produces dry eye by more than one way.
Dry eye is diagnosed mainly by symptoms and confirmed by tests,9 which assess the tear film profile. In this study an attempt is made to assess the magnitude of the problem of dry eye in patients attending the eye clinic by administering a standard questionnaire and subjecting them to tests assessing the tear film profile.
Aim Of The Study
1) To study the tear film profile, prevalence and epidemiology of dry eye in patients attending the eye clinic.
2) To find out the etiology of dry eye in these patients.
METHODS
Patients attending the eye clinic of Sur and B. Ali hospitals between March 1, 2002 to March 31, 2002 were included in the study. The total number of patients studied was 127. In all these patients a standard questionnaire was administered. Then these patients were subjected to TBUT (Tear breakup time), assessment of tear meniscus, detailed slit lamp examination of ocular surface to look for blepharitis, spks, filaments, mucous plaques, symblepharon, bitot spots and so on. At the end, each of these patients was subjected to Schirmer’s test 1. Patients with corneal irregularity or any gross corneal disorders were excluded from the study. Patients with conjunctivitis, chronic dacryocystitis, and corneal ulcerations were also excluded from the study. Reluctant patients were also not involved in the study. In each case the patient was explained about the study and the various tests they would be undergoing and only willing patients were included in the study. When the study was conducted we did not have an ethical committee in our hospital so that formality was not fulfilled.
TBUT:10 Fluorescein dye from a wet fluorescein strip was applied to the lower tarsal plate. Patient is asked to blink and roll eyes around several times. After 1 minute patient is asked to blink once and then hold the eyes open. Time taken in second between the last blink and the appearance of first dry spot in the tear film is recorded. A value of <10 seconds was taken as abnormal. (Sensitivity - 77.8%; specificity 72.4%).11
Schirmers Test 1:10 (measures total reflex and basic tear secretion) to minimize reflex tearing patient is made to sit in a dimly lit room and no ocular medications are instilled. Patient keeps his eye open during the test. The amount of wetting of standard whatman filter paper strip kept at the junction of medial 2/3 and Lateral 1/3 of the lower lid margin after 5 minutes was measured and recorded. A >/= 15mm is taken as normal. (Sensitivity - 76.9%; specificity - 72.4%).11
Statistical Analysis: The data obtained from the study was analyzed using 95% level of confidence at 5 % significance level.
RESULTS
A total of 127 patients were included in the study, 41.73 % (95% CI: 33.1 to 50.3%) patients were <30 years and 58.27% (95% CI: 49.7 to 66.9) were >30 years. Table 1 30.77% (95% CI: 30.8 to 47.9%) were males and 69.23 % (95% CI: 52.1 to 69.1%) were females table 2.
Table 1: Shows Distribution of Patients According to Age
|
Age in years |
Number |
% |
|
<30 |
53 |
41.73% |
|
>30 |
74 |
58.27% |
Table 2: Shows Distribution of Patients According to Sex
|
Gender |
Number |
% |
|
Male |
50 |
30.37% |
|
Female |
77 |
60.63% |
Of the 127 cases 5.51% (95% CI: 1.5% to 9.5%) had abnormal schirmers, 22.83 % (95% CI: 15.5% to 30.1%) had abnormal tear breakup time and 14.17% (95% CI: 8.1 % to 20.2%) had abnormal schirmers and TBUT. A total of 42.5 % (95% CI: 33.9 to 51.1%) cases had abnormality in either schirmers or TBUT or both.
(Table 3)
When tear film profile was compared with gender it was found that abnormal schirmers was found more in females (5 of 77 cases) than males (2 of 50 cases), abnormal TBUT was found more in males 28% ( 95% CI: 15.5 to 40.4%) as against females 19.5% ( 95% CI: 10.6 to 28.3%) and both abnormalities were found equally in both sexes 14% (95% CI: 4.38 to 23.6% in males and 6.47 to 22.1% in females). Overall 40.3% (95%CI 29.3 to 25.2%) females and 46% (95% CI: 32.2 to 59.8%) males in the study showed abnormality in one or the other tear film tests. Thus a significant difference in tear film abnormality was seen in case of TBUT (males > females - 28% vs. 19.5 %) and females outnumbered males (31 females vs. 23 males) when overall abnormalities were considered. (Table 3)
Table 3: Shows Distribution of Sex According to the Abnormalities in Tear Film Profile
|
Gender |
Abnormal
Schirmers |
Abnormal
TBUT |
Abnormal BUT
+
Schirmers |
Total |
|
Male |
2
(4%) |
14
(28%) |
7
(14%) |
23 (46%) |
|
Female
|
5
(6%) |
15
(19.5%) |
11
(14%) |
31 (40.3%) |
|
Total |
7(5.51%)
|
29(22.83%)
|
18(14.17%)
|
54(42.5%) |
When tear film profile was compared in cases < 30 years and those above 30 years, it was observed that abnormal schirmers was found in 5.7% (95% CI: 0.5 to 11.8%) of cases <30 years as against 5.4% (95% CI: 0.26 to 10.56%) in > 30 years. Abnormal TBUT was found more often in cases > 30 years i.e 32.4% (95% CI: 21.7 to 43.1%) as against 9.4% (95% CI: 1.56 to 17.3%) in < 30 years. Abnormalities in both schirmers and TBUT was also seen more frequently in > 30 years of age 18.9% (95% CI: 10.0 to 27.8%) as compared to < 30 years 7.5% (95% CI: 0.44 to 14.6). Overall abnormality was found more in older individuals > 30 years - 56.75% (95% CI: 45.5 to 68.05) than in young i.e < 30 years - 22.6 % (95% CI: 11.3 to 33.9%). Thus cases above > 30 years of age showed significant abnormalities in TBUT and both schirmers and TBUT as compared to younger age group. The overall tear film abnormality was found in older individuals (56.75%; 95% CI: 45.47 to 68.0%) as against younger age group 22.6 % (95% CI: 11.3 to 33.9%). (Table 4)
Table 4: Shows Distribution of Age According to Abnormalities of Tear Film Profile
|
Age in
years |
Abnormal
Schirmers |
Abnormal
BUT |
Abnormal BUT
+
Schirmers |
Total |
|
<30 |
3
(5.7%) |
5
(9.4%) |
4
(7.5%) |
12
(22.6%) |
|
>30 |
4
(5.4%) |
24
(32.4%) |
14
(18.9%) |
42
(56.75%) |
When tear film profile was examined in patients with diseases causing dry eye or on drugs causing dry eye it was seen that 28.6% (95% CI: 5.0 to 62.04%) cases of abnormal schirmers had trachoma while 37.8% (95% CI: 22.27 to 55.6%) cases of abnormal TBUT had trachoma and 44.3% (95% CI: 21.48 to 67.4%) cases with combined abnormality of TBUT and schirmers had trachoma. Overall about 21 cases 38.8% (95% CI: 25.89 to 51.89%) with abnormal tear film profile had trachoma. Other diseases did not figure prominently in cases with abnormal tear film profile. As regards to drugs, although individually none of the tests were shown to be abnormal significantly, overall about 16.7 (95% CI: 6.73 to 26.6%) cases with any type of abnormality showed some relation to drugs. Surgery was not found to occur significantly in any case showing tear film abnormality. Thus, trachoma was prominent among diseases causing tear film abnormality. Drugs causing dry eye to some extent was shown to cause dry eye in this study. (Graph 1)
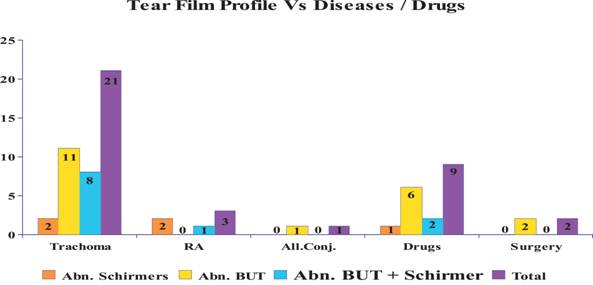
Graph 1: Shows the Distribution of Various Diseases and Other Causes of Dry Eye in Patients with Abnormal Tear Film Profile
When symptoms in cases of abnormal tear film profile was analyzed, burning was seen in 2 cases (28.5%) with abnormal schirmers, 7 cases (24%) in cases with abnormal TBUT and 4 cases (22%) with combined abnormality and overall 13 cases 24% (95% CI: 12.67 to 35.5%). Itching /Irritation was seen in none of the cases with abnormal schirmers, 5 cases (17%) with abnormal TBUT, 4 cases (22%) with combined abnormality and overall 9 cases 16.5% (95% CI: 6.73 to 26.61%). Other symptoms were negligible. Thus burning followed by itching/irritation was seen in fairly significant number of cases of patients with abnormal tear film profile. (Graph 2)
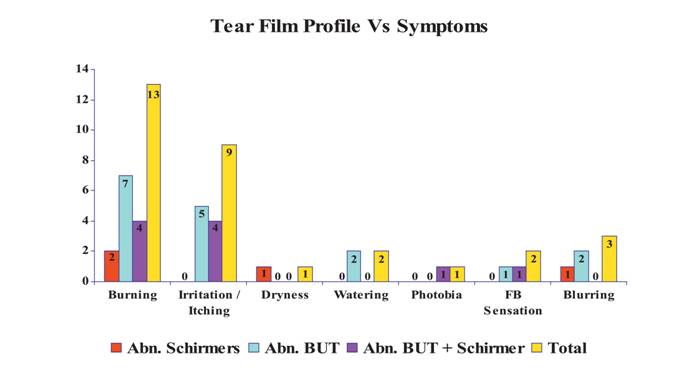
Graph 2: Shows Patients Symptoms in Cases of Abnormal Tear Film Profile
DISCUSSION
This is a pilot project and a short term study. This study is the first study on tear film status/dry eye in Oman. Since trachoma was the major eye problem two decades ago and now we are facing the sequelae to this apart from other conditions causing dry eye we were prompted to undertake this study. Dry eye is a far too common a disorder seen in ophthalmic practice presenting with myriad of symptoms and signs which the clinician too often misses to diagnose resulting in under diagnosis of the condition.12 This results in patient’s frustration as he is not relieved of symptoms and seeks help from another doctor and thereby ends up developing side effects due to over medication or preservatives in the drops and serious conditions like c.ulcers and glaucoma. So, in this study an attempt has been made to find out the magnitude of the problem in patients visiting eye clinic, their sex, age distribution and the common symptomatology they present with and what causes this problem so that patients with dry eye are not missed out in the busy clinic.
In this study of the 127 patients, 50 were males 30.37% (95% CI: 30.87 to 47.87%) and the rest were females showing that there was a fair representation of sexes in the study. As regards to age 41.73% (95% CI: 33.1 to 50.3%) were < 30 years and 58.27% (95% CI: 49.7 to 66.9%) were > 30 years of age, also showing that the two groups are fairly well represented.About 42.5 % (95% CI: 33.9 to 51.1%) in this study showed abnormality in tear film tests namely TBUT and/or Schirmers. A Canadian study in optometric practice showed 25% of the patients had dry eye symptoms.13 In a population based survey by Sahai et al.,14 the prevalence was found to be 18.4%. It is lower than what is found in our study probably because the study was population based which included normal individuals also and the number was larger.
While an Australian study, which was population based showed 16.3% prevalence,15 when tested by schirmers test alone. Our study showed a prevalence of 5.51% when schirmers alone was considered. The difference in the results were probably due to the fact that in our set up the most common cause of dry eye is trachoma which affects the goblet cells and not the lacrimal gland so the tear secretion may be normal while in Australia the cause may be immunological (Sjogrens) which mainly affects the lacrimal gland and hence produce abnormal schirmers. When tear film profile was compared in males and females, females showed higher frequency of abnormal schirmers, TBUT and both together as compared to males although not significant. When the overall picture was visualized it was seen that females clearly out numbered males in terms of absolute numbers (31 females vs. 23 males) while in terms of proportion/percentage males marginally dominated (46% [95% CI: 32.2 to 59.8%] males vs. 40.3% [95% CI: 29.3 to 51.2%] females). In several studies, namely Sahai et al.14 Sendecka et al.,16 to name a few, females clearly out numbered males. In our study also females out numbered males in absolute numbers but when individual test of tear function were analyzed it was seen that there was only a marginal difference. Population based study may help us to overcome this problem.
Tear film profile except schirmers alone was found to be abnormal more often in older age groups (> 30 years) than in younger age group and was found to be significant 56.75% (95% CI: 45.47 to 68.0%) in > 30 years vs. 22.6% (95% CI: 11.3 to 33.9% in < 30 years). This conforms to a study by Sahai et al. who found increased dry eye prevalence in age groups 31 - 40 years and > 75 years.14 Another study by Brewitt et al. showed that about 20% of individuals aged > 40 years experienced dry eye symptoms.17 The increased frequency of abnormality in tear film tests in older age groups in our study can be explained in part by the fact that many of them had old trachomatous lesions in the form of trichiasis with conj scarring which resulted in abnormal TBUT and both schirmers and TBUT. When the diseases that the patients in the study suffered from, relevant to ocular surface were analyzed it was seen that trachoma was observed in 38.8% (95% CI: 25.89 to 51.9%) of the cases with abnormal tear film profile. Trachoma destroys the goblet cells and produces mucin deficiency as evidenced by the fact that 37.8% (95% CI: 20.27 to 55.6%) of cases had abnormal TBUT. Trachoma produces blepharitis and produces abnormal lipid layer resulting in greater evaporation of tears as shown by 44.3% (95% CI: 21.5 to 67.4%) of cases of schirmers and TBUT abnormality having trachoma, and in advanced scarring may obstruct the tear ducts of lacrimal gland leading to aqueous deficiency and block meibomian glands leading to meibomian gland disease.18 Although trachoma was seen in a sizable proportion of patients in this study it is difficult to establish the cause effect relationship in this case. Hitherto no study has attributed trachoma as one of the causes. Sahai et al., has mentioned excessive wind, smoking, and sunlight exposure as few of the risk factors but trachoma did not figure in their study.14 Sandecka et al. mentions Rheumatoid arthritis as the main disease causing dry eye.16 No other diseases supposed to cause dry eye figured significantly in this study. Only 3 patients had Rheumatoid arthritis and 1 patient had allergic conjunctivitis. About 9 (16.7%) patients in our abnormal tear film profile had applied/consumed one drug or the other which was likely to cause dry eye of whom 6 cases were with abnormal TBUT but again the number is not significant and can’t establish any cause effect relationship in this case. No study so far has studied drugs, as one of the risk factors and a larger study is required to identify drugs as one of the risk factors of dry eye.
A lack of correlation between dry eye symptoms and signs like schirmers, TBUT and so on, has been seen. So an attempt was made in this study to see whether the above observation was true or not. In this study it was found that 24% (95% CI: 12.67 to 35.4%) of the patients with abnormal tear film profile had burning as the chief symptom followed by irritation and itching in 16.5% (95% CI: 6.73 to 26.61%) and other symptoms like feeling of dryness, foreign body (FB) sensation, photophobia and blurring were found in a negligible proportion of patients with abnormality in tear film. Thus we see that even in our study there were a considerable number of patients 65 % (95% CI: 56.7 to 73.3%) are without any symptoms. In a study by Nichols et al. the results showed lack of correlation between dry eye tests and symptoms.18 In another study by Begley et al. it was found that the dry eye symptoms correlated moderately with symptoms and very poorly with clinical signs.19 To sum up, it has been seen that there is no strong correlation between symptoms and clinical signs and tear film tests. Thus, one can infer from this observation that patients can remain compensated despite abnormalities found in tear film tests. This lack of correlation makes the significance of tear film test questionable to some extent.
CONCLUSION
Large number of patients had abnormal tear film profile most of them were asymptomatic. Females showed tear film abnormality more often than males. Aged individuals showed abnormalities in tear film profile more often than younger age group. Trachoma figured prominently amongst the diseases in cases with abnormal tear film profile.
ACKNOWLEDGEMENTS
I would like to thank the nurses and optometrists of the eye departments of Sur and B. Ali hospitals of South Sharqiya region who have helped us in conducting the study. Last but not least, I am extremely grateful to the patients who cooperated with us to undergo the various tests performed by us during the study.
“This paper was presented in “dry eye symposium” held in connection with Muscat month in April 2002”
REFERENCES
-
McCarty CA, Basak AK, Livingston PM, Stainslavsky YL, Taylor HR. The epidemiology of dry eye in Melbourne Australia Ophthalmology 1998; 105:1114-1119
-
Schein OD, Munoz B, Tielsch JM, Bandeen-roche K, West S Prevalence of dry eye among the elderly. Am J ophthalmol 1997; 124:723 728
-
Lekhanont K, Rojanaporn D, Chuck RS, Vongthongsri A. Prevalence of dry eye in Bangkok,Thailand. Cornea 2006; 259:1162-1167
-
Lin Pei-YU PY .prevalence of dry eye among elderly Chinese population in Taiwan: The shipai eye study. Ophthalmology 2003; 110: 1096 1101
-
Ferris RL, Stuchell RN, Nisngard R. Sjogrens’s syndrome and keratoconjunctivitis sicca. Cornea 1991; 10:207-209
-
Toda I. Lasik and Dry eye. Compr Ophthalmol Update 2007; 8:79-85
-
Reddy M, Reddy PR, Reddy SC. Conjunctival impression cytology in dry eye states. Indian J Ophthalmol 1991; 39:122 124.
-
Bron AJ, Tifany JM. Contribution of meibomian gland disease to dry eye. Ocul Surf 2004; 2:149-165
-
Roche KA. Self-reported assessment of dry eye in population based setting Invest Ophthalmol Vis Sci 1997; 38:2469-2475
-
Sandeep Saxena. Clinical practice in ophthalmology 2003;2930
-
Vitali C, Mountsopaulos HM, Bombardieri S. The European study group on diagnostic criteria for Sjogrens syndrome, sensitivity and specificity of tests for ocular and oral investigation in Sjogrens syndrome Ann. Rheum. Dis. 1994; 53:637-647
-
Schein OD, Munoz B, Tielsch JM. Prevalence of dry eyeamong the elderly. Am J Ophthalmol 1997; 124:723-728
-
Doughty MJ, Fonn D, Richter D. A patient questionnaire approach to estimating the prevalence of dry eye symptoms in patients presenting to optometric practices across Canada. Optom Vis sci 1997;74:624 631
-
Sahai A, Malik P. Indian J Ophthalmol 2005; 53:87-91
-
McCarty CA, Bansal AK, Livingston PM. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology 1998; 105:1114-1119
-
Sandecka M, Baryluk A. Prevalence and risk factors of dry eye syndrome Przegl epidemiol 2004; 58:227-233
-
Brewitt H, Sistani F. Dry eye disease: The scale of the problem. Surv Ophthalmol 2001; 45:199-202
-
Nichols KK, Nichols JJ. The lack of association between signs and symptoms in patients with dry eye disease. Cornea 2004; 23:762-770
-
Begley CG, Chalmers RL, Abetz L, Venkatraman K. The relationship between habitual patient-reported symptoms and clinical signs among patients with dry eye of varying severity Invest Ophthalmol Vis Sci. 2003; 44:4753-4761
|
|