Pain is an important health problem which is frequently encountered in a primary care setting. It has been identified to be the main reason behind 40% of the visits made to primary care physicians.1 Acute pain has an essential biological value since it warns the individual about an underlying disease process or pathology.2 For example, a patient who complains of sudden right lower abdominal pain could have acute appendicitis. It is very easy, in such circumstances, to correlate pain as a symptom with physical signs and specific diagnostic tests. However, it becomes more complex and challenging when physicians deal with chronic pain because of the absence of any typical physical signs and the lack of definite diagnostic tools. Other contributing factors include the subjective nature of pain, its multidimensional nature, and the lack of effective treatment.3 Such unique features are illustrated in the International Association for the Study of Pain (IASP)’s definition, which describes pain as an “unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage”.4 The arbitrary period for acute pain to become chronic is defined as three months, which is the maximum period usually allowed for “normal tissue healing time” to occur.4 In chronic pain, the focus is usually on rehabilitation and improving quality of life unlike the case with acute pain where the focus is on finding a cure.3
Chronic pain is a major health problem which affects a large number of the world’s population.5 Epidemiological studies have demonstrated that up to 45% of the populations of some countries are affected.5 Chronic pain is significantly associated with high morbidity and mortality.6,7 It can lead to devastating effects at the individual level leading to loss of function, unemployment, and inability to perform routine daily activities.8 In extreme cases, it might cause disability.9 Psychologically it can lead to poor self-esteem and depression.7,10 Indeed, studies showed that almost half of patients who suffered from chronic pain were also suffering from concurrent depression.11 Chronic pain is associated with a heavy socioeconomic burden.8 The cost of pain to any health care system is tremendous since it does not only include direct costs associated with doctors’ visits, investigations, and medications, but it also includes indirect costs such as lost wages and loss of productivity.8
Previous studies have shown that chronic pain is more prevalent in women, and that prevalence increases with age.10 An association between chronic pain and other comorbid medical conditions, particularly cardiovascular diseases and depression, has also been reported.10,12 The majority of patients with chronic pain are usually seen in a primary health care setting in most countries.13 Studies conducted on these patients in a primary care setting are therefore of great importance as such studies might help to improve the identification of these patients and might lead to an improvement in management strategies. A limited number of studies have addressed the demographic and clinical characteristics of chronic pain patients in the Middle East.14,15 Hence, this study aimed to identify the demographic and clinical characteristics of chronic pain patients who presented to a primary health care setting in Oman.
Methods
This cross-sectional study was conducted at Sultan Qaboos University Health Center, Muscat, Oman. Data for all patients (≥ 18 years) attending the general Family Medicine clinics over a period of one year (1 January 2010 to 31 December 2010) were retrieved from the electronic Hospital Information System. Out of this sample, all patients who were prescribed any of the following analgesics: paracetamol, diclofenac, celecoxib, tramadol, amitriptyline, gabapentin, and co-codamol for a minimum period of three consecutive months were identified using the pharmacy records. The diagnosis of chronic pain was verified by reviewing the clinical notes of each of those identified patients and by conducting telephonic interviews with each patient from the chronic pain group. Patients who were found to be taking any of the analgesics for any other purpose rather than chronic pain were excluded. The first and second author were responsible for collecting the data and conducting the telephonic interviews.
The following demographic characteristics were collected: age, gender, and nationality (Omani nationals and non-Omani). In addition, the following clinical data were collected from the electronic medical records: (1) body mass index (BMI), (2) type of chronic pain condition: osteoarthritis (OA), low back pain, migraine, post-traumatic, headache, and others (neck and shoulder pain, elbow pain, chronic fatigue syndrome, fibromyalgia, facial pain, and neuropathic pain), (3) comorbidities: diabetes mellitus, hypertension, ischemic heart disease (IHD), obesity, depression, gastritis, thyroid disease and dyslipidemia, and (4) type of analgesic prescribed: diclofenac, amitriptyline, celecoxib, tramadol, paracetamol, gabapentin, and co-codamol.
An age- and gender-matched control group of patients with no chronic pain was created. Patients in this group were randomly selected by using a random number table from the remaining total of 6 368 patients who did not have chronic pain.
Descriptive statistics were used to describe the data. For categorical variables, frequencies and percentages were reported. Differences between groups were analyzed using Pearson’s chi-square tests (or Fisher’s exact tests for cells < 5). For continuous variables, mean and standard deviation (SD) were used to summarize the data. Analyses were performed using Student’s t-test. An a priori two-tailed level of significance was set at 0.05. Statistical analyses were conducted using Stata version 13.1 (STATA Corporation, College Station, TX, USA).
Ethical approval was obtained from the Research and Ethics Committee of the College of Medicine and Health Sciences, Sultan Qaboos University, Muscat, Oman.
Results
A total of 6 609 were included in the study. The overall mean age of the subjects was 41.0±14.0 years, and 58.9% (n = 3 898) were women. A total of 241 (3.6%) patients were identified to have chronic pain according to our study criteria. The majority of the subjects were females (n = 174; 72.1%). A significantly higher proportion of female patients had chronic pain compared to their male counterparts (4.5% vs. 2.5%; p < 0.001). Females with chronic pain were also found to be younger compared to males (53.0±12.0 vs. 57.0±14.0; p = 0.012). The proportion of Omani nationals was found to be significantly higher in cases of chronic pain compared to the control group (83.4% vs. 70.1%; p < 0.001).
Although BMI values were not documented for a significant proportion of the patients (n = 102; 42.3% of the case group, n = 84; 35.2% of control group), subjects with chronic pain were found to have significantly higher BMI compared to the control group (31.0±6.0 vs. 28.0±6.0 kg/m2; p < 0.001). Chronic pain was found to be significantly associated with the following comorbidities: diabetes (33.1% vs. 20.7%; p < 0.001), obesity (35.2% vs. 26.5%; p = 0.001), and hypertension (51.0% vs. 38.5%; p = 0.002). The prevalence of IHD and depression were also noted more commonly among chronic pain patients, but the relationship was not statistically significant. Table 1 summarizes the characteristics of chronic pain patients compared to the control group.
Table 1: Demographic and clinical characteristics of the chronic pain group compared to the control group.
|
Age, mean ± SD, years |
54.0 ± 13.0 |
54.0 ± 13.0 |
Matched |
|
Male sex |
67 (27.8) |
67 (27.8) |
Matched |
|
Omani national |
201 (83.4) |
169 (70.1) |
< 0.001 |
|
Diabetes |
80 (33.1) |
50 (21.7) |
< 0.001 |
|
Hypertension |
123 (51.0) |
93 (38.5) |
0.002 |
|
BMI |
31.0 ± 6.0 |
28.0 ± 6.0 |
< 0.001 |
|
IHD |
15 (6.2) |
9 (3.7) |
0.263 |
|
Depression |
10 (4.1) |
3 (1.2) |
0.092 |
|
Gastritis |
6 (2.4) |
5 (2.0) |
1.000 |
|
Asthma |
6 (2.4) |
11 (4.5) |
0.332 |
|
Thyroid |
12 (4.9) |
19 (7.8) |
0.265 |
|
Dyslipidemia |
70 (28.9) |
65 (26.9) |
0.668 |
*Data presented as n (%) unless otherwise specified.
SD: standard deviation; BMI: body mass index; IHD: ischemic heart disease.
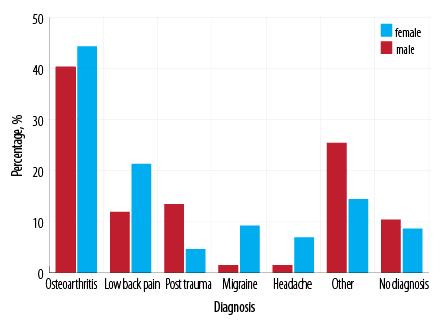
Figure 1: Conditions causing chronic pain among patients in the chronic pain group and variation according to sex.
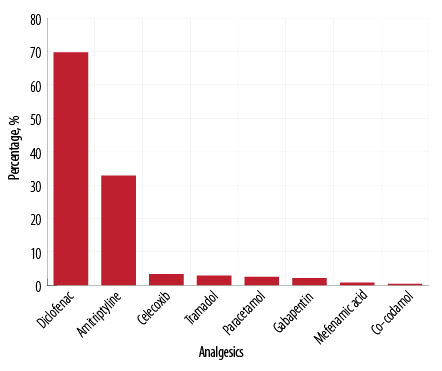
Figure 2: Types of analgesics used by patients with chronic pain.
OA was the commonest pain condition (n = 104; 43.1%) for the whole group followed by low back pain (n = 45; 18.6%). These two conditions were also the commonest among females affecting 44.2% (n = 77) and 21.2% (n = 37), respectively, followed by migraine (n = 16; 9.1%). Males had a higher prevalence of post-traumatic pain (n = 9; 13.4%). Some patients suffered from two pain conditions concurrently [Figure 1].
The majority of patients were on diclofenac (n = 168; 69.7%) or amitriptyline (n = 79; 32.8%). Some patients were taking two or more analgesics simultaneously [Figure 2].
Discussion
Chronic pain was more prevalent in specific groups of patients, namely, females, who were relatively younger compared to their male counterparts, Omani nationals, and obese individuals. Chronic pain was also more commonly associated with other common chronic diseases such as diabetes and hypertension. The two most commonly pain conditions seen in our study population were OA and low back pain. Nonsteroidal anti-inflammatory drugs (NSAIDs) were the most frequently prescribed class of medications.
Epidemiological data from 10 developed and seven developing countries using a common survey questionnaire indicated that women were more commonly affected with chronic pain.10 Fillingim et al,16 who had reviewed several epidemiological studies to address the sex-related influences on pain concluded that women were at substantially greater risk for many clinical pain conditions. An American internet-based survey on a nationally representative sample of 35 718 individuals demonstrated that females had a higher prevalence of pain than males (34% vs. 27%, respectively).17 A Norwegian study based on a mailed questionnaire concluded that women reported chronic pain more frequently than men, and their pain intensity scores were significantly higher than those reported by men.18 Two studies which were conducted in the Gulf region, also reported similar findings.14,15
The preponderance of females over males could be mainly due to the well-documented gender differences in pain perception which makes females more sensitive to pain compared to males.16,19 Interestingly, gender differences in pain persisted even in experimentally induced pain which manifested as greater pain sensitivity, enhanced pain facilitation, and reduced pain inhibition in females.16 Multiple mechanisms have been postulated for these gender differences which include existing biological variations in the nociceptive and perceptual pain systems, genetic factors, sex hormones, psychosocial factors such as sex role beliefs, and pain-coping strategies.16,19
The literature indicates a definite relationship between chronic pain and age. There is generally a higher prevalence of chronic pain in older age.17,20,21 Reitsma et al,22 using data from seven cross-sectional cycles in the National Population Health Survey and the Canadian Community Health Survey, which covered the period of years from 1994 to 2008, reported that chronic pain was most prevalent among the oldest age group (65 years and older) and women. Andersson et al,23 also reported an increased prevalence of pain with age particularly during the years from 50 to 59 for both genders. Kaki studied 1 686 patients in Saudi Arabia and identified the 50–59 year age group as the group mainly affected.15 The finding of the latter study is consistent with our results in terms of the mean age of those affected with chronic pain (53 for females, and 57 for males). However, our finding that females were affected at a younger age compared to males is contrary to that of Deeny et al,14 who reported that women were affected at an older age in their study (45 vs. 41 years). The difference could be attributed probably to genetic and cultural factors.
Moreover, our results indicated that Omani nationals were affected more significantly with chronic pain compared to non-Omanis. This finding is consistent with the literature which confirmed the association of chronic pain with ethnicity.24,25 Ahn et al,26 had illustrated this association by demonstrating that Asian-American participants with knee OA had significantly higher levels of clinical pain intensity as well as significantly higher experimental pain sensitivity compared to non-Hispanic white participants. A study from Kuwait had similarly reported a higher prevalence of chronic pain in Kuwaiti nationals compared to non-Kuwaitis.14 Possible other reasons for our finding besides ethnicity could be accounted for by the predominance of sedentary lifestyle in Oman and other Gulf countries and the lack of routine physical activity due to cultural and environmental factors.
The findings of our study showed that the mean BMI was significantly higher in the chronic pain group compared to the control group. Several studies documented a positive correlation between chronic pain and BMI.21,27,28 As yet, the causal relationship between the two remains unclear.27 Obesity is hypothesized to lead to pain because of excessive mechanical stresses and its proinflammatory state.27 It is also recognized that chronic pain may lead to decreased physical activity due to fear of exacerbating pain and this often results in weight gain.27,28 Genetic, psychological and metabolic factors may also lead to both obesity and pain.27,28
Comorbidities, which included hypertension and diabetes, were significantly associated with chronic pain in our study. Similar findings were reported by Deeny et al,14 who found a higher prevalence of comorbid medical problems among patients who had chronic pain. The relationship between pain and hypertension is of great clinical interest, but is poorly understood.29 Researchers evaluated a large sample of 10 135 participants for both the prevalence of hypertension and blood pressure-related hypoalgesia by measuring their resting blood pressure and pain sensitivity.30 The researchers concluded that chronic pain was significantly associated with comorbid hypertension and higher chronic pain intensity
was a significant predictor of positive hypertension status beyond the effects of traditional demographic risk factors.30
Although, it is widely recognized that diabetic patients are commonly affected with neuropathic type of pain as a complication of the disease itself, some researchers have suggested a possible independent relationship between glucose control and chronic pain.31,32 In a cross-sectional study of a predominantly black American population of 417 with diabetes, participants who reported pain were more than twice as likely to have high glycosylated hemoglobin levels (> 8.0%).32
OA and low back pain were the two commonest types of pain in our study population. Our findings are similar to other studies conducted in other countries.10,17,23 Moreover, the literature also showed that specific pain conditions were commonly seen in one specific gender. For instance, women were reported to be affected more commonly with pain in the neck, shoulder, arm, and thigh compared to men.23 Other conditions that predominantly affect females include fibromyalgia, migraine and chronic tension-type headache, irritable bowel syndrome, temporomandibular disorders, and interstitial cystitis.16 Our study showed a higher prevalence of OA and low back pain among females. Elliott et al,33 had similarly reported a higher prevalence of OA in women, but contrary to our results they found a higher prevalence of back pain in men.
Our results showed that NSAIDs were the commonest class of analgesics prescribed. A large-scale telephone survey of 15 European countries showed that the most common prescription medications taken by respondents were NSAIDs, followed by weak opioid analgesics, and paracetamol.34 Other studies also reported similar results.35 The use of NSAIDs has been associated with serious adverse effect such as gastrointestinal hemorrhage, renal impairment, and hepatic toxicity.36 Thus, strategies for rational prescribing including prescription of alternative analgesics with better safety profile particularly in the elderly population who are at higher risk for adverse effects should be implemented.37
Our study has several limitations. The design of the study as cross-sectional has its own inherent limitations. The study population does not represent the general population due to the fact that the study was done at a university health center, which serves a specific patient population and is not open to the general public. Pharmacy records were used to identify patients with chronic pain, which is not an ideal method to identify patients but was the only method available. It is possible that other medications could have been missed as patients could have bought some of their other pain medications over the counter. Moreover, this problem would have an impact on the ability to determine the prevalence of drug use, but this was not considered as one of the objectives of the study. Documentation of essential information such as BMI was missing or incomplete for many patients, which could have affected the findings.
Conclusion
Female gender and ethnicity were found to be significant demographic variables among chronic pain patients in a primary care setting in our study. Comorbidities, such as hypertension and diabetes, were more prevalent in patients with chronic pain. The most common types of chronic pain were OA and low back pain. The commonest classes of analgesics prescribed were NSAIDs. Despite the limitations of our study, the findings were consistent with the published literature. Future studies should aim to determine the prevalence of chronic pain, and those utilizing a larger sample size and conducted in community-based primary health care centers are needed to develop better understanding of this important clinical condition.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. Mäntyselkä P, Kumpusalo E, Ahonen R, Kumpusalo A, Kauhanen J, Viinamäki H, et al. Pain as a reason to visit the doctor: a study in Finnish primary health care. Pain 2001 Jan;89(2-3):175-180.
- 2. Schug SA. 2011–the global year against acute pain. Anaesth Intensive Care 2011 Jan;39(1):11-14.
- 3. Mills S, Torrance N, Smith BH. Identification and management of chronic pain in primary care: A review. Curr Psychiatry Rep 2016 Feb;18(2):22.
- 4. International Association for the Study of Pain (IASP) taxonomy [cited 2017 March]. Available from: http://www.iasp-pain.org/Taxonomy#Pain.
- 5. Smith BH, Torrance N. Epidemiology of chronic pain. In: McQuay HJ, Moore RA, editors. Systematic reviews in pain research: methodology refined. Seattle: IASP Press; 2008.
- 6. Torrance N, Elliott AM, Lee AJ, Smith BH. Severe chronic pain is associated with increased 10 year mortality. A cohort record linkage study. Eur J Pain 2010 Apr;14(4):380-386.
- 7. Mäntyselkä PT, Turunen JH, Ahonen RS, Kumpusalo EA. Chronic pain and poor self-rated health. JAMA 2003 Nov;290(18):2435-2442.
- 8. Leadley RM, Armstrong N, Lee YC, Allen A, Kleijnen J. Chronic diseases in the European Union: the prevalence and health cost implications of chronic pain. J Pain Palliat Care Pharmacother 2012 Dec;26(4):310-325.
- 9. Raftery MN, Sarma K, Murphy AW, De la Harpe D, Normand C, McGuire BE. Chronic pain in the Republic of Ireland–community prevalence, psychosocial profile and predictors of pain-related disability: results from the Prevalence, Impact and Cost of Chronic Pain (PRIME) study, part 1. Pain 2011 May;152(5):1096-1103.
- 10. Tsang A, Von Korff M, Lee S, Alonso J, Karam E, Angermeyer MC, et al. Common chronic pain conditions in developed and developing countries: gender and age differences and comorbidity with depression-anxiety disorders. J Pain 2008 Oct;9(10):883-891.
- 11. Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med 2003 Nov;163(20):2433-2445.
- 12. Fayaz A, Watt HC, Langford RM, Donaldson LJ. The association between chronic pain and cardiac disease: A cross-sectional population study. Clin J Pain 2016 Dec;32(12):1062-1068.
- 13. Gureje O, Von Korff M, Simon GE, Gater R. Persistent pain and well-being: A World Health Organization study in primary care. JAMA 1998 Jul;280(2):147-151.
- 14. Deeny MC, Al Hamdan E, Ross EL, Edwards RR, Huang CC, Jamison RN. Chronic pain, comorbid medical conditions, and associated risk factors in Kuwait: Gender and nationality differences. Pain Med 2015 Nov;16(11):2204-2211.
- 15. Kaki AM. Pain clinic experience in a teaching hospital in Western, Saudi Arabia. Relationship of patient’s age and gender to various types of pain. Saudi Med J 2006 Dec;27(12):1882-1886.
- 16. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL III. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain 2009 May;10(5):447-485.
- 17. Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain 2010 Nov;11(11):1230-1239.
- 18. Rustøen T, Wahl AK, Hanestad BR, Lerdal A, Paul S, Miaskowski C. Prevalence and characteristics of chronic pain in the general Norwegian population. Eur J Pain 2004 Dec;8(6):555-565.
- 19. Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth 2013 Jul;111(1):52-58.
- 20. Azevedo LF, Costa-Pereira A, Mendonça L, Dias CC, Castro-Lopes JM. Epidemiology of chronic pain: a population-based nationwide study on its prevalence, characteristics and associated disability in Portugal. J Pain 2012 Aug;13(8):773-783.
- 21. Sjøgren P, Ekholm O, Peuckmann V, Grønbaek M. Epidemiology of chronic pain in Denmark: an update. Eur J Pain 2009 Mar;13(3):287-292.
- 22. Reitsma ML, Tranmer JE, Buchanan DM, Vandenkerkhof EG. The prevalence of chronic pain and pain-related interference in the Canadian population from 1994 to 2008. Chronic Dis Inj Can 2011 Sep;31(4):157-164.
- 23. Andersson HI, Ejlertsson G, Leden I, Rosenberg C. Chronic pain in a geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clin J Pain 1993 Sep;9(3):174-182.
- 24. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain 2015 Aug;16(8):769-780.
- 25. Hardt J, Jacobsen C, Goldberg J, Nickel R, Buchwald D. Prevalence of chronic pain in a representative sample in the United States. Pain Med 2008 Oct;9(7):803-812.
- 26. Ahn H, Weaver M, Lyon DE, Kim J, Choi E, Staud R, et al. Differences in clinical pain and experimental pain sensitivity between Asian Americans and Whites with knee osteoarthritis. Clin J Pain 2017 Feb;33(2):174-180.
- 27. Okifuji A, Hare BD. The association between chronic pain and obesity. J Pain Res 2015 Jul;8:399-408.
- 28. Hitt HC, McMillen RC, Thornton-Neaves T, Koch K, Cosby AG. Comorbidity of obesity and pain in a general population: results from the Southern Pain Prevalence Study. J Pain 2007 May;8(5):430-436.
- 29. Saccò M, Meschi M, Regolisti G, Detrenis S, Bianchi L, Bertorelli M, et al. The relationship between blood pressure and pain. J Clin Hypertens (Greenwich) 2013 Aug;15(8):600-605.
- 30. Olsen RB, Bruehl S, Nielsen CS, Rosseland LA, Eggen AE, Stubhaug A. Hypertension prevalence and diminished blood pressure-related hypoalgesia in individuals reporting chronic pain in a general population: the Tromsø study. Pain 2013 Feb;154(2):257-262.
- 31. Liberman O, Peleg R, Shvartzman P. Chronic pain in type 2 diabetic patients: a cross-sectional study in primary care setting. Eur J Gen Pract 2014 Dec;20(4):260-267.
- 32. Herbert MS, Varley AL, Andreae SJ, Goodin BR, Bradley LA, Safford MM. Association of pain with HbA1c in a predominantly black population of community-dwelling adults with diabetes: a cross-sectional analysis. Diabet Med 2013 Dec;30(12):1466-1471.
- 33. Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA. The epidemiology of chronic pain in the community. Lancet 1999 Oct;354(9186):1248-1252.
- 34. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006 May;10(4):287-333.
- 35. Clark JD. Chronic pain prevalence and analgesic prescribing in a general medical population. J Pain Symptom Manage 2002 Feb;23(2):131-137.
- 36. Carson JL, Willett LR. Toxicity of nonsteroidal anti-inflammatory drugs. An overview of the epidemiological evidence. Drugs 1993;46(Suppl 1):243-248.
- 37. Atkinson TJ, Fudin J, Pandula A, Mirza M. Medication pain management in the elderly: unique and underutilized analgesic treatment options. Clin Ther 2013 Nov;35(11):1669-1689.