| Introduction
An estimated 10% of the world’s population experiences some form of disability or impairment.1 Despite the increase in the prevalence of disability worldwide, not much attention has been paid to its evaluation, management and prevention.2
Neuropsychiatric disorders are one of the major contributors to the global burden of disease and disability.3 The disability in various neuropsychiatric disorders is reflected in multiple domains including the ability to perform everyday tasks and to achieve normal functional milestones such as work, stable social relationships, and living independently.4
According to the International Classification of Impairment, Disability and Handicap (ICIDH); disability is the interference with activities of the whole person in relation to the immediate environment.5 According to the Census of India (2001), 2.13% of the total population of India is suffering from some form of disability.6 In contrast, the National Sample Survey Organization (NSSO) has estimated that the number of persons with disabilities in India is 1.8% of the Indian population.7 However, both these agencies concur that disability due to mental disorders constitutes about 10% of total disability in the country.
As per the National Sample Survey of 2004, 94 people per 100, 000 population were found to be mentally retarded and 105 people per 100, 000 population suffered some form of mental illness.8 The concept of disability has increasingly been seen as a social rather than individual impairment. However, it is estimated that only 2% of people with disabilities in developing countries have access to rehabilitation and the appropriate basic services.
The Persons with Disabilities (Equal Opportunities, Protection of Rights and Full Participation) Act, 1995 has been enacted by the government of India for the benefit of such population. It extends to the whole of India except the State of Jammu and Kashmir. Six medical conditions leading to disability, including mental illness and mental retardation, come under the purview of the act.
Various tools have been developed to assess disability. These include WHO-Disability Assessment Schedule (WHODAS), WHO Short Disability Assessment Schedule (WHODAS-S), Activities of Daily Living (ADL) Index, International Classification of Functioning, Disabilities and Health (ICF), International Classification of Functioning, Disabilities and Health (ICF) for children and adolescents (ICF-CY), Global Assessment of Functioning (GAF) scale and Schedule for the Assessment of Psychiatric Disability (SAPD). The Indian Disability Evaluation and Assessment Scale (IDEAS) developed by The Rehabilitation Committee of Indian Psychiatric Society has been approved by the government of India to assess disability due to psychiatric disorders.9
The issue of disability in psychiatric disorders has been studied extensively in Indian setting.9-17 However, there are no reports on the profile of those seeking disability certificates in the country. Assessment of disability levels in out-patient, in-patient or community based samples helps establish the epidemiological parameters of psychiatric disability. However, it does not provide any insights into the profile of patients making utilisation of such certification for the purpose of availing disability benefits. Such a study would help understand the ground reality with regards to utilization of disability evaluation services by the psychiatric patients in India. This is the first study of its kind to the best of our knowledge that reports findings from such a clinical cohort in India.
Methods
The study was carried out in the Department of Psychiatry of a tertiary care multispecialty teaching hospital. A chart review of the records of the patients referred for disability evaluation over a one year period from April 2009 to March 2010 was conducted. The department is a designated nodal point for issuing disability certificate. The cases claiming disability due to psychiatric disorders are referred to the Department of Psychiatry by the Medical Superintendent of the hospital. Subsequent to registration, the patient is assessed in detail. Assessment is done by a qualified psychiatrist and subsequently confirmed by two other qualified psychiatrists. Information is obtained from the patient, at least one key informant and medical records. First, the diagnosis is established using the ICD-10 (International Statistical Classification of Diseases and Related Health Conditions).18 Subsequently, the disability is assessed using IDEAS. IDEAS is approved by the government of India for documenting the level of disability due to mental illness. It assesses disability under four domains: self care, interpersonal activities (social relationships), communication and understanding, and work. Each item is scored between 0-4, i.e., from no to profound disability, adding scores on 4 items gives the "total disability score."
Global disability score is calculated by adding the "total disability score" and MI2Y score (months in two years - a score ranging between 1 and 4, depending on the number of months in the last two years the patient exhibited symptoms). Global disability score of 0 corresponds to "no disability," a score between 1-7 corresponds to "mild disability," and a score of 8 and above corresponds to moderate to profound disability.
IDEAS is a well validated instrument and is used across the country for disability evaluation in psychiatric disorders. The alpha value for the scale has been found to be 0.8682, indicating good internal consistency between the items. It has good criterion validity and at face validity. Criterion validity of the scale has been established by comparing IDEAS with SAPD (Schedule for the Assessment of Psychiatric Disability) which has been standardized in India.9
Individuals diagnosed with mental retardation were classified according to the severity level of mental retardation as per the ICD-10 classification.
The records of all the patients referred to the Department of Psychiatry over a one year period were reviewed. All the subjects were included in the analysis. Analysis was carried out using SPSS ver 17.0. Descriptive analysis was carried out for all the subjects. Since the cases with mental retardation are not assessed using IDEAS, the final analysis excluded these cases. All the cases diagnosed with schizophrenia, bipolar affective disorders (BPAD), dementia and obsessive compulsive disorder (OCD) were included in the final analysis. In between group analysis using ANOVA with post hoc analysis was carried out for the duration of illness and IDEAS score for the four neuropsychiatric disorders.
In between group comparisons were carried out for male and female subjects for different socio-demographic variables, IDEAS total score and individuals item score using independent sample t test (parametric test) and Mann Whitney-U test (non parametric test).
Additionally, Spearman’s rank order correlation was calculated to establish the level of correlation between total IDEAS score and score on individual items of the scale. The level of statistical significance was kept at p<0.05 for all the tests.
Conditions of anonymity and confidentiality as recommended in institutional ethical guidelines were strictly adhered to during the course of the study.
Results
A total of 173 subjects were referred to the Department of Psychiatry for disability evaluation. It included 125 (72.3%) males and 48 (27.7%) females. The mean age of the male and female subjects was 28.99 (SD±15.40) years and 28.87 (SD±16.15) years, respectively. The subjects were diagnosed to have been suffering from mental retardation 107 (61.8%), schizophrenia 54 (31.2%), dementia 5 (2.9%), bipolar affective disorder 4 (2.3%) and obsessive compulsive disorder 3 (1.7%) as per the ICD-10. All the subjects except for those having mental retardation were assessed on IDEAS. These cases were included in the final analysis. The socio-demographic profile of these subjects is presented in Table 1.
The 107 cases diagnosed with mental retardation were classified according to the ICD-10 severity level. Fifteen (13.8%) subjects were found to suffer from profound, 40 (37%) from severe, 26 (24.1%) from moderate and 26 (24.1%) from mild mental retardation.
Table 1: Socio-demographic profile of the cases assessed using IDEAS.
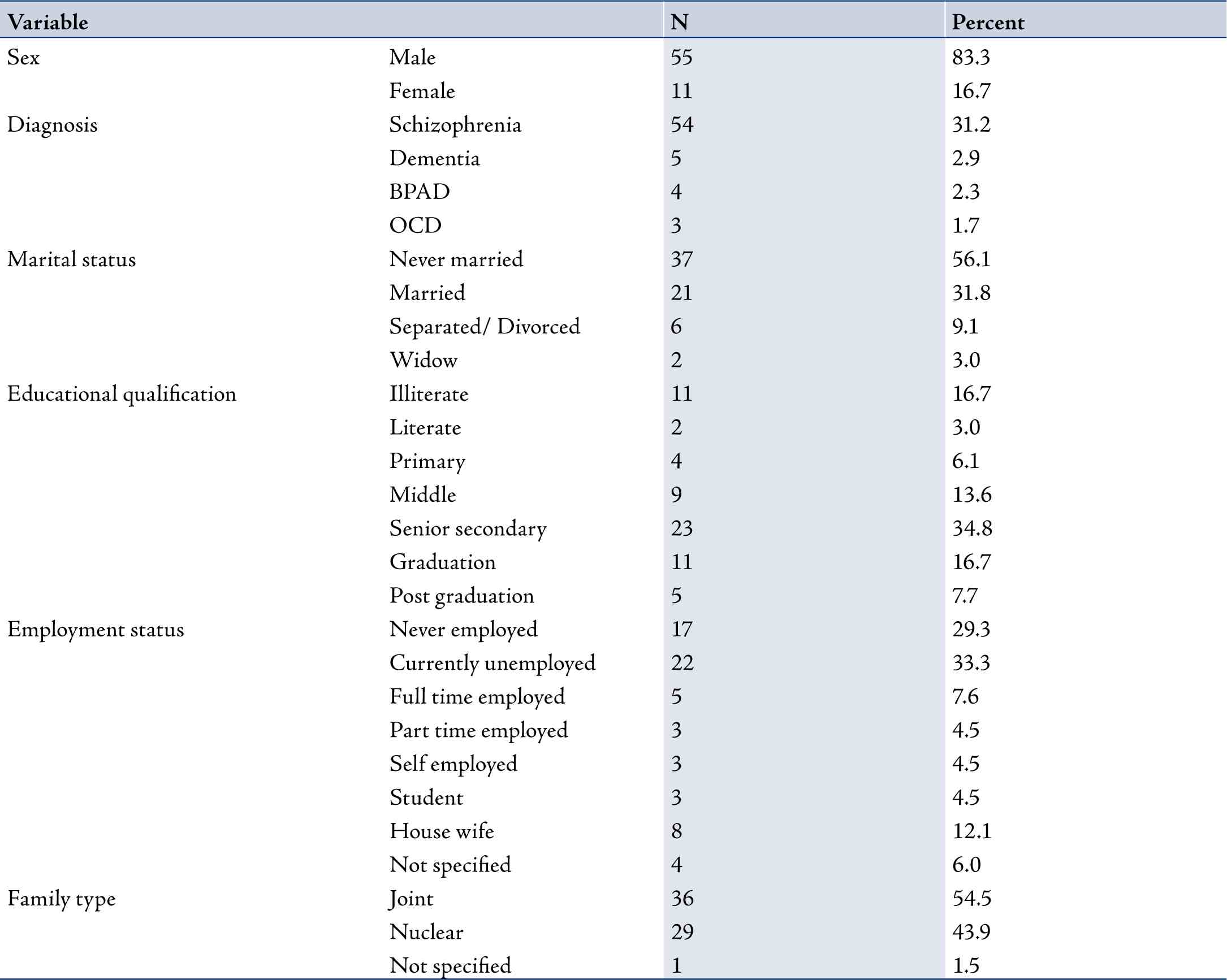
Table 2: In between group analysis for socio-demographic variables
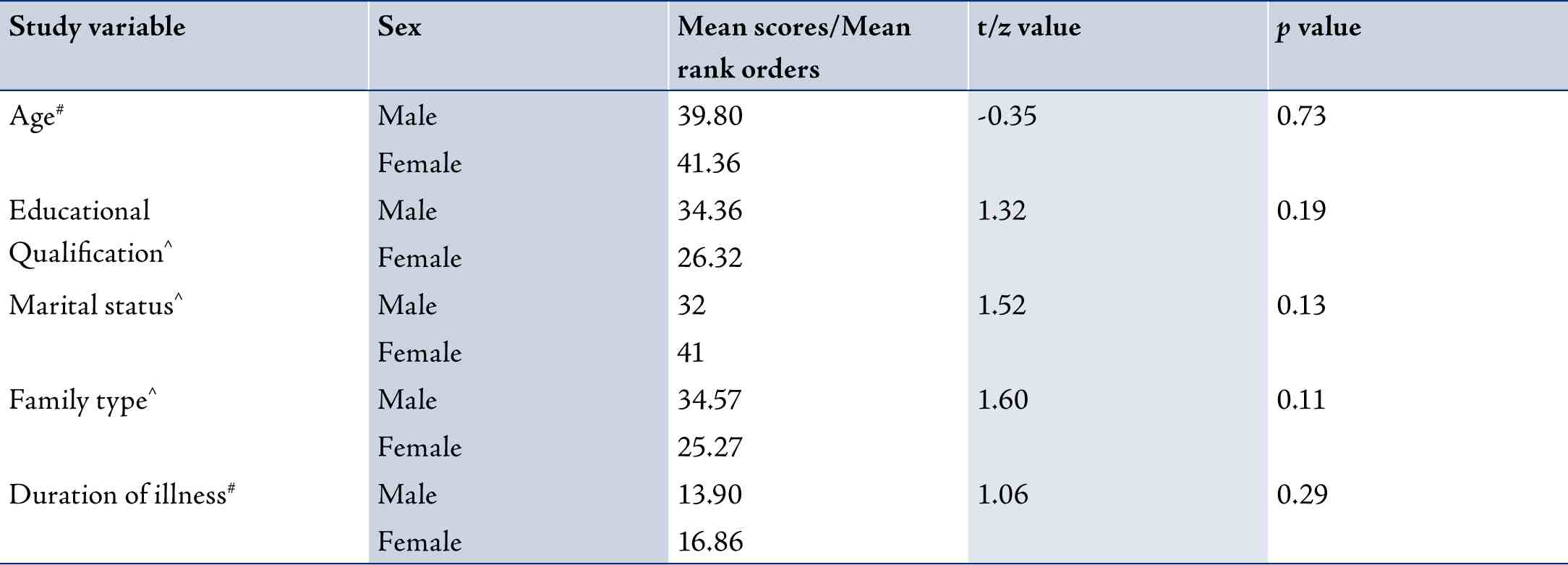
The mean duration of all the psychiatric disorders was comparable in the study sample. Additionally the four disorders did not differ for the gross as well individual item score when analyzed by ANOVA with post hoc analysis. In between group analysis for male and female subjects revealed that the two groups did not differ on various socio-demographic variables including age (t=0.35; p=0.73), educational qualification (z=1.32; p=0.19), family type (z=1.60; p=0.11) and marital status (z=1.52; p=0.13). The two groups were comparable on total duration of illness as well (t=1.06; p=0.29). (Table 2)
Table 3: In between group differences for male and female subjects on IDEAS
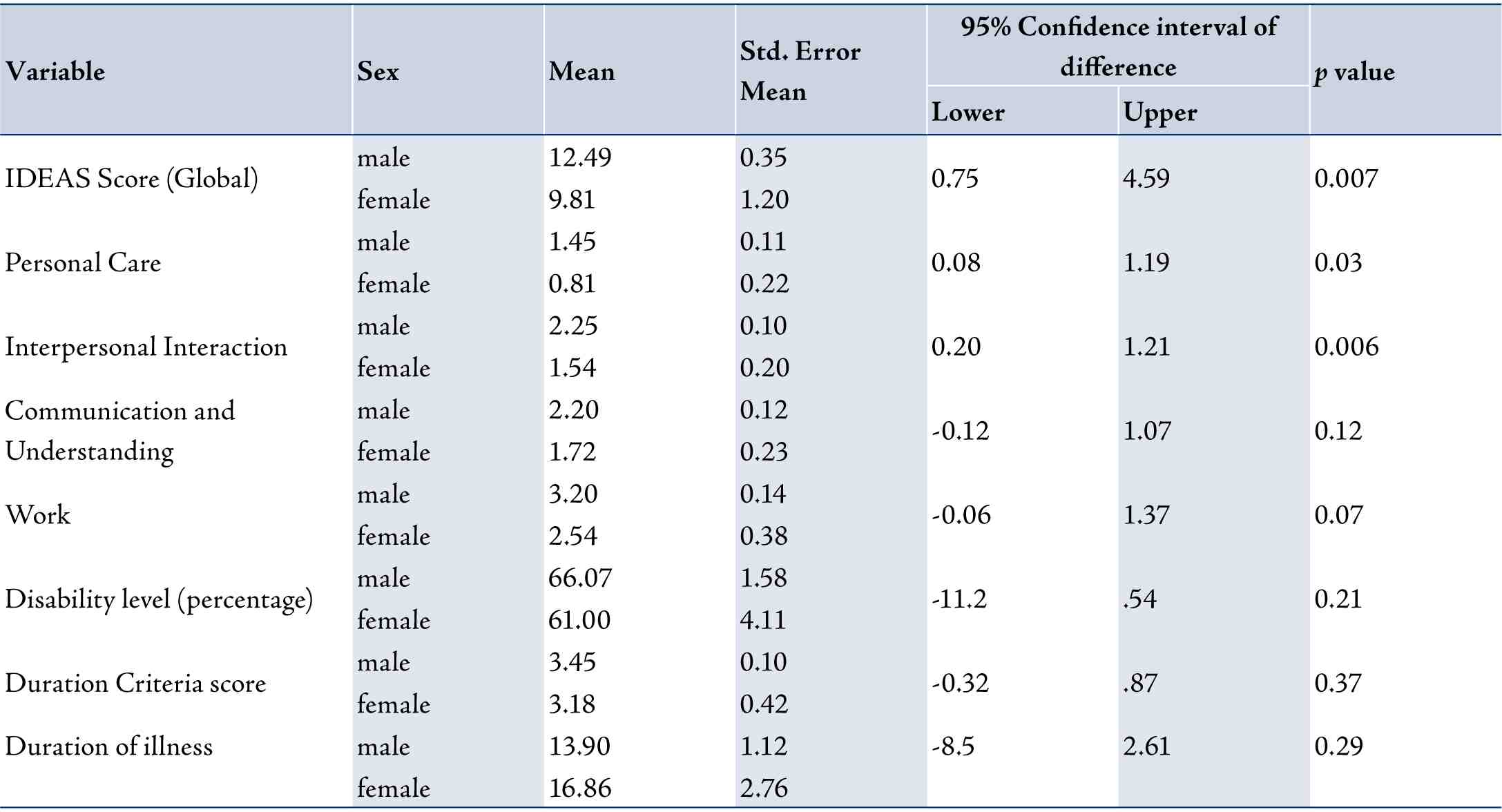
However, male and female subjects differed significantly on the global IDEAS score. The mean scores for the male and female subjects were 12.49 (SD±2.67) and 9.82 (SD±3.96), respectively. Mean scores on different items of IDEAS scale for male and female subjects is given in Table 3. The total score was significantly higher for male subjects compared to female subjects (t=2.78; p=0.007).
The difference was statistically significant for "self care" (t=2.29, p=0.03), and interpersonal activities (social relationships) (t=2.82, p=0.006) items of the scale with male subjects having higher disability scores. However, no significant differences were observed for "communication and understanding" and "work" items.
There was a significant correlation between the global IDEAS score and score on all the items of the scale across all the study subjects. The coefficients of correlation were: r=2.29 for "self care" (p=0.03), r=2.82 for interpersonal activities (social relationships) (p=0.006), r=0.73 for "communication and understanding" (p=0.00) and r=0.59 for "work" )p=0.00).
Discussion
The current study aimed to assess the profile of the patients seeking disability certification for psychiatric disorders in a government designated tertiary care multispecialty hospital. A chart review of all the patients referred to the Department of Psychiatry was carried out by the Medical Superintendent for evaluation purposes. The level of disability has been proposed to be an endophenotypic marker for severe mental illness.19
All the patients except for those suffering from mental retardation were assessed using IDEAS. Our sample had an overwhelming majority of subjects diagnosed with schizophrenia. This is an interesting finding. Studies from the tertiary care hospital out-patient settings in India have reported neurotic stress-related disorders, somatoform disorders and mood disorders to be the most common diagnoses.20,21 Schizophrenia represents a relatively smaller proportion of such cohorts. Findings of overwhelming majority of schizophrenia patients in the current study is a significant finding. Other conditions eligible for benefit under PWD Act, 1995 viz, dementia, BPAD and OCD were markedly underrepresented in the current study.
One possible explanation for this observation could be the fact that schizophrenia is likely to be associated with significant disability in a higher proportion of cases. This finding has been observed in some of the previous Indian studies conducted in tertiary care settings. Hence, in spite of its relatively lower prevalence in the general population, it is overrepresented among those seeking disability certification.
A previous study by Chaudhury et al. (2006) in an out-patient setting in a tertiary care hospital also reported schizophrenia to be the most common contributor to disability (31% of cases).12 BPAD constituted 13%, OCD 11% and dementia 6% of the cases in this study. However, disability due to schizophrenia ranks lower in the community based studies from India.14,15 In a community based study by Kumar et al.14 BPAD and mental retardation constituted 32% and 14% of the total cases, respectively.
Interestingly subjects with schizophrenia, BPAD, dementia and OCD did not differ significantly on the global IDEAS score and scores on individual items of the scale in the current study. Also, the disorders had comparable total duration of illness across the sample. This finding is in contradiction to the usual understanding of schizophrenia being a more disabling condition compared to BPAD and OCD.
Studies from India comparing schizophrenia with BPAD,12 or OCD,9,12 have concluded schizophrenia to be a more disabling condition. However, western studies have reported the disability due to both BPAD,22,23 and OCD,24-26 to be either comparable or even higher than that of schizophrenia. However, one needs to keep in mind relatively smaller sample of BPAD and OCD in our study while drawing inferences.
Another significant finding from the current study is the significant differences observed between male and female study subjects for the gross IDEAS, "self care" and "interpersonal activities (social relationships)" items scores. The scores were significantly higher for male subjects on all the three variables. Additionally, male subjects (72.3%) were disproportionally over represented in our study. This is a reflection of the usual higher proportion of male psychiatric patients being brought to treatment facilities.27,28 Males were overrepresented at 73.3% and 68.4% in the study by Mohan et al. (2005) and Chaudhury et al. respectively.12 Both these studies were conducted in the out-patient setting of a tertiary care hospital.
Literature on gender differences for disability among patients with psychiatric disorders has been controversial. Male psychiatric patients have been found to have higher disability compared to female patients for everyday functioning and social relationships.29 Chaves et al. also found that males had higher levels of disability than females. However, they did not find any differences in social role performance for the two genders.30 Prognosis of schizophrenia has been reported to be better among females compared to males.31 Additionally, longitudinal studies suggest that women with schizophrenia show better social functioning.32 A possible contributor to this observation is the male reticence about disclosing emotional distress that limits their access to support. Female patients have been found to be more likely to belong to joint family in these studies. More support available in joint families has been cited as one of the reasons for lower disability among female patients with schizophrenia.15
However, these earlier studies have been criticised for deriving premature conclusions. Some of the more recent studies have found men with psychiatric disorders to experience disproportionately greater role, social and cognitive disability than women.33 Shankar et al. found the disability to be higher among female subjects compared to male subjects having schizophrenia.10 A more recent study from India by Kujur et al. also found females to be having higher levels of disability on all domains of WHO-DAS (World Health Organisation- Disability Assessment Schedule).34
The current study has certain limitations as well. The findings are from only one centre. One needs to conduct a multicentre study in order to substantiate the findings. Additionally, it would be interesting and informative to analyze the data over subsequent years in order to assess the time trends.
Conclusion
The current study provides an understanding into the disability benefit seeking behavior of psychiatric patients in India. A disproportionately higher proportion of male subjects are seeking disability benefits. This situation warrants appropriate public health interventions in order to ensure more eligible female patients are also receiving these disability benefits. Additionally, the clinicians need to be aware of the fact that patients suffering from BPAD, OCD and dementia might be having disability levels comparable to those suffering from schizophrenia.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
|