Non-communicable diseases are the fastest growing threat to global health and development and economic growth. These conditions are responsible for 63% of deaths worldwide, with half occurring in working-age individuals.1 Diabetes mellitus is one of the leading causes of the increase in non-communicable diseases, with the Middle East being one of the regions with the highest prevalence.2 A key aspect of diabetes control is the prevention of major macrovascular and microvascular complications. Improving glycemic control is one component for reducing complications.3 However, the role of non-glycemic risk factors such as hypertension, hyperlipidemia, and hypercoagulability are additional factors contributing to cardiovascular risk specifically and should be targeted in treatment.4 Cardiovascular diseases (CVDs) include stroke, coronary heart disease, and peripheral vascular disease. More than one-third of the global deaths (37%) are attributed to CVD in patients under the age of 70.5 Without active intervention in managing CVD risk factors, those figures are expected to escalate from 17.5 million deaths per year in 2012 to 22.2 million deaths by 2030.5 In the UAE, a report from the Ministry of Health showed that CVD deaths are a major cause of mortality (specifically myocardial infarction).6 In 2016, the World Health Organization reported that 44% of mortality in the UAE was due to CVD. However, CVD mortality improved between 2000 and 2016, and is expected to improve further until 2025.7
The American Diabetes Association (ADA) has set clear targets for lipid management in patients with diabetes as part of macrovascular risk management presumed to be of atherosclerotic origin.8 Attaining the ADA benchmark in lipid control has always been a global challenge.9–12 The prevalence of diabetes in the UAE is estimated to be 18.98%.2 However, despite this high prevalence, there are few studies evaluating diabetes and its associated risk factors control patterns over the last few years in our region.13–17
The Dubai Health Authority (DHA) is the main governmental health sector in Dubai. The DHA has 13 primary care centers that manage patients with diabetes. Additionally, there are three hospitals with specialized diabetes care departments.
We believe that our study is unique, since the total population of Dubai is just above 2.9 million individuals18 and we have studied around 26 447 patients, which is around 1% of the population. We searched the medical database and included patients with an International Classification of Diseases (ICD) code for diabetes. Moreover, the data included was over five years including all the primary and tertiary care centers in the governmental health sector of Dubai. Those, collectively, would make the outcomes of this study quite robust and has an important epidemiological reflection of the real-life lipids control in patients with diabetes.
Our main aim was to assess lipid control in patients with diabetes across the DHA points of care over five years (2012–2016). Additionally, we aimed to compare the lipid control between primary and tertiary care and between UAE and non-UAE nationals.
Methods
We conducted a retrospective analysis of the electronic medical records of all patients who attended hospitals and primary health care centers in the DHA from January 2012 to December 2016. All patients with an ICD coding of type 1 and 2 diabetes, with or without complications, who had at least one lipids reading per year were suitable for inclusion in the study. Having only one eligibility screening tool, the ICD coding of diabetes may have veiled a large number of patients with diabetes who were coded under other diseases (missed cases), however, at the same time, this gives the study the power of having 100% confirmed diabetes patients, without any inclusion bias.
Since the data was retrospectively collected, we randomly selected the latest lipid panel tests within the fourth quarter in each year, which we thought will reflect the outcome of that particular year, which again led to missing a sizable number of data points if the lipids panel test was not done during that time period (fourth quarter of the year).
Patients were categorized based on the different lipids parameters including total cholesterol (TC), triglycerides (TG), high-density lipoprotein (HDL), low-density lipoprotein (LDL), and non-high-density lipoprotein (non-HDL) levels. All control targets for each lipid parameter were assessed according to the ADA standards,5 since all the study population was patients with diabetes. ADA targets for patients with diabetes to lower cardiovascular risk are < 150 mg/dL for TC, TG < 150 mg/dL, LDL < 100 mg/dL, and non-HDL < 130 mg/dL.8 According to the ADA cutoff points, data was analyzed to obtain the mean of each parameter’s control annually, as well as the percentage of patients at target.
Different variables of lipids panel were further compared between primary versus tertiary services, UAE nationals versus expatriates, and between patients with type 1 versus type 2 diabetes.
Table 1: Demographic distribution of the study population.
|
Males |
12 765 |
48.3 |
|
Females |
13 682 |
51.7 |
|
UAE nationals |
19 508 |
73.8 |
|
Expatriates |
6939 |
26.2 |
|
T1DM |
2625 |
9.9 |
|
T2DM |
23 822 |
90.1 |
|
Tertiary care patients |
10 967 |
41.5 |
|
Primary care patients |
15 480 |
58.5 |
|
DM without CV or renal complications |
24 432 |
92.4 |
UAE: United Arab Emirates; T1DM: type 1 diabetes mellitus; T2DM: type 2 diabetes mellitus; DM: diabetes mellitus; CV: cardiovascular.
Data were statistically described in terms of mean±standard deviation, median and range, or frequencies (number of cases) and percentages when appropriate. Comparison of numerical variables between the study groups was made using Student’s t-test for independent samples in comparing two groups and one-way analysis of variance (ANOVA) test with post-hoc multiple two-group comparisons for comparing more than two groups. Within-group comparison between the different years was made using repeated measures of ANOVA test. For comparing categorical data, the chi-square test was performed. Fisher’s exact test was used instead when the expected frequency was less than five. A p-value < 0.050 was considered statistically significant. All statistical calculations were done using SPSS Statistics (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.).
Table 2: Lipid profile means and percentages in primary and tertiary care and in UAE nationals and expatriates between 2012 and 2016.
|
TC, mg/dL |
170.0 ± 41.5 |
165.0 ± 40.6 |
167.0 ± 41.1 |
168.0 ± 40.9 |
165.0 ± 41.3 |
|
TG, mg/dL |
136.0 ± 92.7 |
131.0 ± 84.2 |
133.0 ± 88.5 |
131.0 ± 89.6 |
140.0 ± 91 |
|
HDL, mg/dL |
49.0 ± 13.2 |
50.0 ± 14.0 |
49.0 ± 13.6 |
51.0 ± 13.9 |
46.0 ± 12.2 |
|
LDL, mg/dL |
99.0 ± 36.2 |
92.0 ± 34.8 |
96.0 ± 35.5 |
96.0 ± 35.5 |
96.0 ± 35.8 |
|
LDL, < 100 mg/dL, % |
56.0 |
65.0 |
60.5 |
61.1 |
58.9 |
|
2012 |
52.9% |
62.6% |
31.2% |
35.5% |
60.9% |
|
2013 |
59.6% |
65.6% |
36.4% |
39.4% |
67.0% |
|
2014 |
59.5% |
67.2% |
35.8% |
41.6% |
66.2% |
|
2015 |
52.5% |
63.7% |
33.4% |
39.7% |
60.7% |
UAE: United Arab Emirates; TC: total cholesterol; TG: triglycerides; HDL: high-density lipoprotein; LDL: low-density lipoprotein;
non-HDL: non-high-density lipoprotein.
Results
A total of 26 447 patients with diabetes were included in this analysis; the male to female distribution was similar (48.3% and 51.7%, respectively). Being a governmental sector (where all nationals receive free treatment), 73.8% of patients in our cohort were Emirati nationals (n = 19 508), while expatriates were only 26.2% (n = 6939). As expected, type 1 diabetes mellitus patients made up to 9.9% (n = 2625) of the cohort [Table 1].
In total, amongst both primary and tertiary care patients, the mean values of all lipid profile components over the study duration was within the target range as per the ADA standards of care [Table 2]. Interestingly, around 60.5% of patients achieved an LDL < 100 mg/dL [Figure 1]. Tertiary care patients achieved a mean LDL of 92.0±34.8 mg/dL while in primary care the mean was 99.0±36.2 mg/dL. We noted a statistical difference in the LDL targets achieved between patients attending tertiary versus primary care centers (p < 0.001). Sixty-five percent of patients in tertiary care had an LDL < 100 mg/dL compared to 56.0% of patients in primary care [Figure 2].
UAE nationals had higher TC levels compared to expatriates (168.0±40.9 mg/dL and 165.0±41.3 mg/dL, respectively). However, their TG levels over the five years were lower than expatriates (131.0±89.6 mg/dL and 140.0±91.0 mg/dL, respectively). Interestingly, mean LDL was similar in UAE nationals and expatriates (96.0±35.5 mg/dL and 96.0±35.8 mg/dL, respectively), despite the higher TC in UAE nationals [Table 2]. This might be attributed to higher HDL levels in UAE nationals compared to expatriates, which was statistically significant (p < 0.001).
The non-HDL cholesterol (non-HDL-C) of < 130 mg/dL was achieved in 67.9% in tertiary care in 2012 compared to 60.9% in primary care, and this difference was statistically significant (p < 0.001) [Table 2]. Reassuringly, tertiary care centers achieved tighter lipids indices across the study period, which may be attributed to looking after patients at higher risk of CVD.
The non-HDL cholesterol (non-HDL-C) of < 130 mg/dL was achieved in 67.9% in tertiary care in 2012 compared to 60.9% in primary care, and this difference was statistically significant (p < 0.001) [Table 2]. Reassuringly, tertiary care centers achieved tighter lipids indices across the study period, which may be attributed to looking after patients at higher risk of CVD.
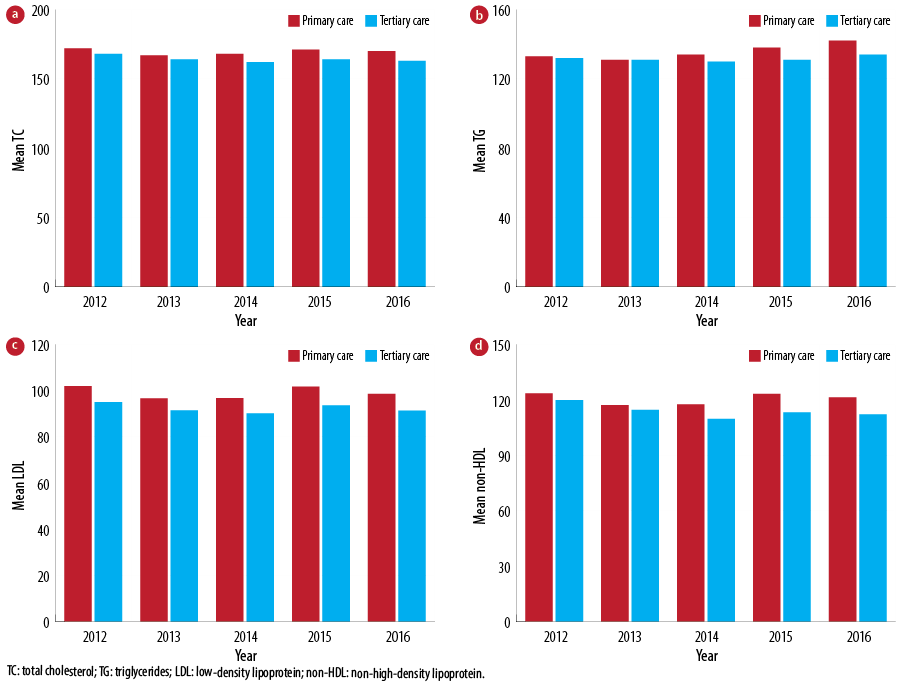
Figure 1: Mean lipid parameter control between primary and tertiary care centers across the study duration (2012–2016).
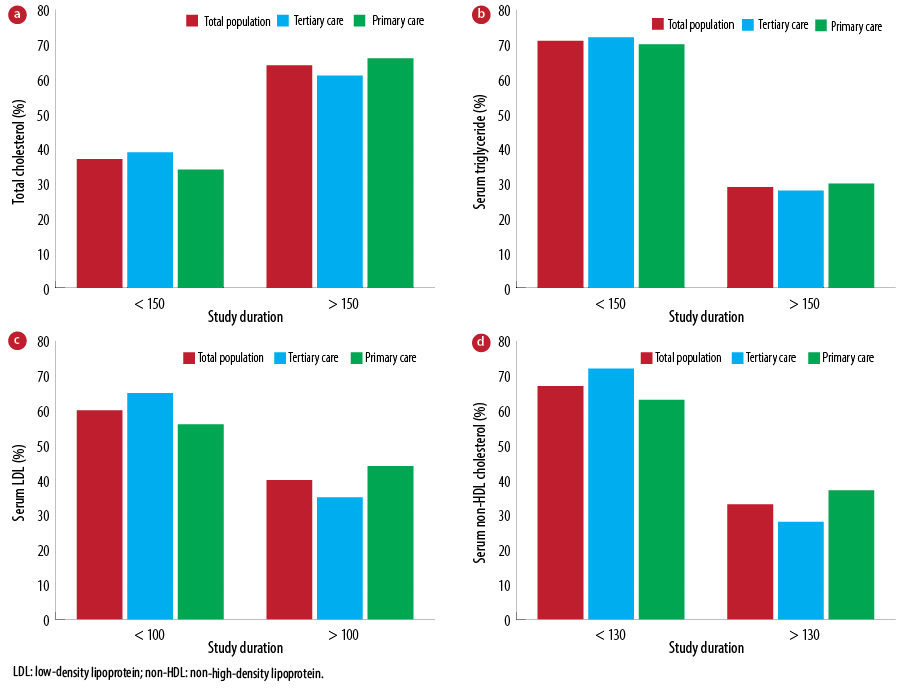
Figure 2: Percentage of patients with target lipid parameter control between primary and tertiary care centers across the study duration (2012–2016).
Discussion
CVD is a leading global cause of morbidity and mortality amongst patients with diabetes.5 In the Middle East, the volume of CVD deaths is one of the highest in the world.19
Diabetes is associated with a two- to four-fold increased risk for CVD and is considered a coronary artery disease (CAD) risk equivalent.20 LDL-cholesterol (LDL-C) appears to have the major role in atherosclerosis and CAD development, and, hence, its management may take precedence over glycemic reduction to reduce CAD risk in individuals with diabetes. Surprisingly, despite the benefits of treating dyslipidemia in both primary and secondary prevention of CVD, a significant number of patients do not achieve their target lipid levels in many countries, particularly those patients at higher CVD risk.21–25
The ADA has put forth specific guidelines and LDL targets for patients with diabetes as they constitute a high-risk category. However, achieving those targets is a formidable task.8
Our review includes 26 447 patients with diabetes making it the largest cohort of patients evaluated for diabetes and lipid control at both primary and tertiary levels in the UAE and the Middle East region.13,14,26–29 Sixty-five percent of our patients in tertiary care had an LDL < 100 mg/dL compared to 56.0% of patients in primary care. This might be explained by the fact that patients attending tertiary care are mostly high-risk groups who are targeted to lower their LDL levels.
The Centralized Pan-Middle East Survey on the under-treatment of hypercholesterolemia (CEPHEUS) using lipid-lowering drug therapy included 5276 patients in six Arabian Gulf countries (Bahrain, Saudi Arabia, Qatar, Oman, Kuwait, and the UAE). LDL-C goal was attained in 52% of the cohort according to the updated National Cholesterol Education Program, Adult Treatment Panel-III. However, the CEPHEUS did not have a separate analysis of patients with diabetes.30
On the other hand, results from the Dyslipidemia International Study-Middle East, in which more than three-quarters of patients were classified as very high-risk (based on European Society of Cardiology guidelines) demonstrated that the most prevalent lipid abnormality, despite chronic statin treatment, was elevated LDL-C levels. Goal LDL-C levels
(< 70 mg/dL) were not attained in 61.8% of all patients and 69.5% of very high-risk patients, which included a cohort of patients with diabetes.26
In our cohort, 60.5% of patients achieved a target LDL < 100 mg/dL. Similar results were reported in another retrospective cohort study in Dubai, which found 71% of patients met the LDL targets.17 The study analyzed the patterns of care and treatment target success in patients with diabetes. However, the study population was only 250 patients selected from a single tertiary care setup over six months, which minimizes the reliance on these figures from an epidemiological point of view. Moreover, the patients selected were only Emirati nationals. Our study included 6939 non-Emirati patients giving a better epidemiological estimate.
In tertiary care, patients achieved a mean LDL level of 92.0 mg/dL while in primary care the mean was 99.0 mg/dL. This might be explained by the fact that patients attending tertiary care are mostly high-risk groups who are targeted to lower LDL levels. Nonetheless, in both levels of care, patients were able to achieve desirable mean LDL levels.
Non-HDL-C levels < 130 mg/dL were achieved in 67.9% of patients in tertiary care in 2012 compared to 60.9% in primary care (p < 0.001). Non-HDL-C is gradually gaining the attention of the guidelines, and calculating non-HDL has become a recommended routine in the dyslipidemia management.8,31
Although UAE nationals had higher TC compared to expatriates, their TG levels over the five years were lower. We do not have a specific explanation for this observation, but perhaps the dietary habit and lifestyle may play a role. Interestingly, the mean LDL mean was similar in UAE nationals and expatriates, despite the higher TC in UAE nationals. This might be attributed to higher HDL levels in UAE nationals compared to non-nationals, which was statistically significant (p < 0.001).
This study may have a valuable impact on health strategies and health economics regulations since we were able to evaluate five years of data from a huge number of confirmed diabetes mellitus cases. Moreover, this study calls for further efforts to improve physicians’ and patients’ awareness of dyslipidemia management in diabetes. Additionally, based on this data, short and long-term non-communicable diseases strategic plans need to include this data as an important estimate of the volume of the problem and to replicate similar studies to track the change.
Our data missed the detailed patient record including the duration of diabetes, and the stage of underlying cardiovascular or renal disease, being retrospectively captured data from the electronic record. Our data were derived from different centers within the same healthcare authority in a single emirate. The study does not describe the medications background and the patients’ compliance details. Hence, the issue of whether we need to focus on physicians inertia or patients’ awareness still needs to be unveiled.
Conclusion
This is the largest epidemiological analysis in the region. The percentage of patients with diabetes across the DHA primary and tertiary health care centers achieving lipid targets is amongst the highest reported in the region and, perhaps, globally. There were significantly better lipid control indices achieved in tertiary care compared to primary care. Such studies need to be routinely replicated to boost physician-patient efforts in improving the
lipids parameters.
Disclosure
The authors declared no conflicts of interest. No funding was received for this study.
references
- 1. World Economic Forum. The global economic burden of non-communicable diseases. Harvard School of Public Health. September 2011.
- 2. International Diabetes Federation (IDF). Diabetes Atlas 5th edition, 2014 Update.
- 3. Nathan DM; DCCT/EDIC Research Group. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care 2014;37(1):9-16.
- 4. Dluhy RG, McMahon GT. Intensive glycemic control in the ACCORD and ADVANCE trials. N Engl J Med 2008 Jun;358(24):2630-2633.
- 5. World Health Organization. Global Health Observatory Data Repository; 2016. [cited June 2019]. Available from: http://www.apps.who.int/gho/data/node.main.A859?lang=en.
- 6. Ministry of Health and Prevention. United Arab Emirates; 2015 Report.
- 7. World Health Organization - Noncommunicable Diseases (NCD) Country Profiles. 2018. [cited June 2019]. Available from: http://www.who.int/nmh/countries/are_en.pdf.
- 8. Professional Practice Committee. Professional practice committee: Standards of medical care in diabetes-2018. Diabetes Care 2018 Jan;41(Suppl 1):S3-S3.
- 9. Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA 2004 Jan;291(3):335-342.
- 10. Leiter LA, Berard L, Bowering CK, Cheng AY, Dawson KG, Ekoé JM, et al. Type 2 diabetes mellitus management in Canada: is it improving? Can J Diabetes 2013 Apr;37(2):82-89.
- 11. Ong KL, Cheung BM, Wong LY, Wat NM, Tan KC, Lam KS. Prevalence, treatment, and control of diagnosed diabetes in the U.S. National Health and Nutrition Examination Survey 1999-2004. Ann Epidemiol 2008 Mar;18(3):222-229.
- 12. Khunti K, Ceriello A, Cos X, De Block C. Achievement of guideline targets for blood pressure, lipid, and glycaemic control in type 2 diabetes: A meta-analysis. Diabetes Res Clin Pract 2018 Mar;137:137-148.
- 13. Afandi B, Malik AA, AlKaabi J, Elhouni A, Aziz F. Clinical diabetes care of patients with type 2 diabetes at a major tertiary care hospital in the United Arab Emirates. J Diabetes Metab Disord Control 2015;2(1):7-12.
- 14. Afandi B, Ahmad S, Saadi H, Elkhumaidi S, Karkoukli MA, Kelly B, et al. Audit of a diabetes clinic at Tawam hospital, United Arab Emirates, 2004-2005. Ann N Y Acad Sci 2006 Nov;1084:319-324.
- 15. Reed RL, Revel AO, Carter A, Saadi HF, Dunn EV. A clinical trial of chronic care diabetic clinics in general practice in the United Arab Emirates: a preliminary analysis. Arch Physiol Biochem 2001 Jul;109(3):272-280.
- 16. Shehab A, Elnour A, Abdulle A. A clinical audit on diabetes care in patients with type 2 diabetes in Al-ain, United arab emirates. Open Cardiovasc Med J 2012;6:126-132.
- 17. Osenenko KM, Szabo SM, Qatami L, Korenblat Donato BM, Al Madani AA, Al Awadi FF, et al. Patterns of care and treatment target success among persons with type 2 diabetes mellitus in Dubai: A retrospective cohort study. Value Health Reg Issues 2015 Sep;7:87-93.
- 18. Dubai Statistics Centre report 2017. [cited June 2019]. Available from: https://www.dsc.gov.ae/en-us/Pages/dubainfigure-details.aspx.
- 19. Ramahi TM. Cardiovascular disease in the Asia Middle East region: global trends and local implications. Asia Pac J Public Health 2010 Jul;22(3)(Suppl):83S-89S.
- 20. Haffner SM; American Diabetes Association. Dyslipidemia management in adults with diabetes. Diabetes Care 2004 Jan;27(Suppl 1):S68-S71.
- 21. EUROASPIRE. A European society of cardiology survey of secondary prevention of coronary heart disease: principal results. EUROASPIRE Study Group. European Action on Secondary Prevention through Intervention to Reduce Events. Eur Heart J 1997 Oct;18(10):1569-1582.
- 22. EUROASPIRE II Study Group. Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries; principal results from EUROASPIRE II Euro Heart Survey Programme. Eur Heart J 2001 Apr;22(7):554-572.
- 23. Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among US adults: findings from the National Health and Nutrition Examination Survey, 1999 to 2000. Circulation 2003 May;107(17):2185-2189.
- 24. Pearson TA, Laurora I, Chu H, Kafonek S. The lipid treatment assessment project (L-TAP): a multicenter survey to evaluate the percentages of dyslipidemic patients receiving lipid-lowering therapy and achieving low-density lipoprotein cholesterol goals. Arch Intern Med 2000 Feb;160(4):459-467.
- 25. Frolkis JP, Pearce GL, Nambi V, Minor S, Sprecher DL. Statins do not meet expectations for lowering low-density lipoprotein cholesterol levels when used in clinical practice. Am J Med 2002 Dec;113(8):625-629.
- 26. Al Sifri SN, Almahmeed W, Azar S, Okkeh O, Bramlage P, Jünger C, et al. Results of the dyslipidemia international study (DYSIS)-middle east: Clinical perspective on the prevalence and characteristics of lipid abnormalities in the setting of chronic statin treatment. Kirchmair R, ed. PLoS ONE. 2014;9(1):e84350.
- 27. Leiter LA, Berard L, Bowering CK, Cheng AY, Dawson KG, Ekoé JM, et al. Type 2 diabetes mellitus management in Canada: is it improving? Can J Diabetes 2013 Apr;37(2):82-89.
- 28. Ong KL, Cheung BM, Wong LY, Wat NM, Tan KC, Lam KS. Prevalence, treatment, and control of diagnosed diabetes in the U.S. National Health and Nutrition Examination Survey 1999-2004. Ann Epidemiol 2008 Mar;18(3):222-229.
- 29. Khunti K, Ceriello A, Cos X, De Block C. Achievement of guideline targets for blood pressure, lipid, and glycaemic control in type 2 diabetes: A meta-analysis. Diabetes Res Clin Pract 2018 Mar;137:137-148.
- 30. Arafah M, Al-Hinai AT, Al Mahmeed W, Al-Rasadi K, Al Tamimi O, Al Herz S, et al. Centralized pan-middle east survey on the undertreatment of hypercholesterolemia results from the CEPHEUS study in Arabian Gulf Countries. Angiology; 65(10):919-926.
- 31. Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, et al. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil 2007 Sep;14(Suppl 2):S1-S113.