A 39-year-old premenopausal woman presented with complaints of persistent pain in her lower abdomen lasting one year. She had history of exploratory laparotomy two years prior for tubercular pyoperitoneum. She completed her course of antitubercular medication and remained asymptomatic in the intervening period (around 10 months). She then developed pain, abdominal distension, and constipation. An abdominal examination revealed a midline scar. Her abdomen was soft and non-tender. It appeared distended below the umbilicus, more in the left iliac fossa than the right. An ill-defined abdominopelvic mass was palpable in the lower abdomen. Rectovaginal examination also suggested fullness in the rectouterine pouch. Ultrasonography (USG) of the abdomen demonstrated a large anechoic abdominopelvic cystic mass extending from the left lower quadrant of the abdomen deep in the pelvis into the rectouterine pouch. The left ovary appeared normal but adhered to the uterus posteriorly. The right ovary was visualized separately and was normal. Contrast-enhanced computed tomography (CECT) scan, which was performed for further characterization of the cystic mass and its relation to adjacent anatomic structures. CECT revealed displacement of bowel loops by a well-defined irregularly loculated fluid collection measuring 23 × 12 × 20 cm in the left paracolic gutter and the pelvis [Figure 1]. Both the ovaries appeared normal on CECT and transvaginal USG. Serum CA-125 was 9.2 U/mL. USG guided aspiration of the cystic mass yielded clear fluid. The fluid protein was 4.8 g%, sugar 92 mg% and fluid was negative for acid-fast bacilli on Ziehl–Neelsen staining. Adenosine deaminase activity level in the fluid was 14.0 U/L. Fluid cytology revealed a few reactive
mesothelial cells.
Question
- What is your diagnosis?
a. Tubercular loculated ascites.
b. Peritoneal inclusion cyst.
c. Ovarian carcinoma.
d. Mesenteric cyst.
Answer
b. Peritoneal inclusion cyst.
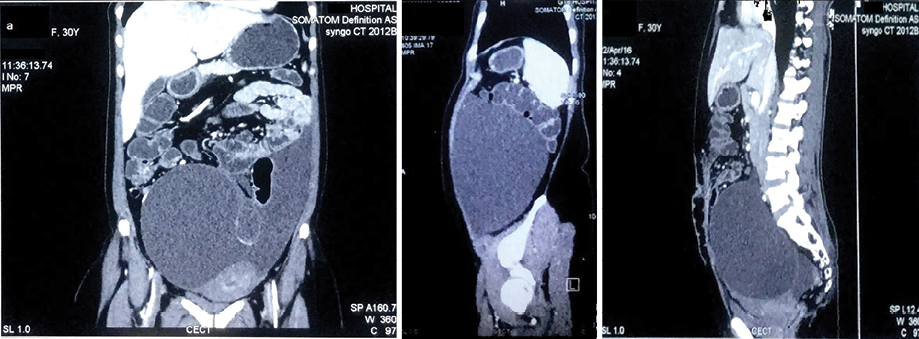
Figure 1: Contrast-enhanced computed tomography scan displays a well-defined irregularly loculated fluid collection measuring 23 × 12 × 20 cm in the left paracolic gutter and pelvis.
Discussion
Peritoneal inclusion cysts are aggregates of variable sized, fluid-filled, mesothelial-lined cysts of the abdominopelvic cavity, usually found in reproductive age women with a history of abdominal or pelvic surgeries or inflammation. The serous fluid is derived from the ovarian stroma. Normally, this fluid is absorbed by the peritoneum, but the absorptive capacity may be compromised as a result of surgery, trauma, or inflammation. Moreover, post-surgical adhesions can lead to formation of a complex cystic pelvic mass with septations. Although the etiology and nature of the disease process are not well understood, it is believed that functional, active ovaries and adhesions are essential for the development of peritoneal inclusion cyst, which is upheld by presentation of this disease after the onset of puberty in females. However, it is also known to occur in men, with a reported incidence up to 17%.1 The fluid is thought to be secreted by the visceral peritoneum.
The usual presentation of peritoneal inclusion cysts is progressive lower abdominal or pelvic pain. Infrequently, the woman complains of backache, constipation, urinary frequency or retention, anorexia, dysfunctional uterine bleeding, or infertility. The risk factors for developing the disease include previous intraperitoneal surgeries, intraperitoneal inflammation, pelvic inflammatory disease, peritoneal tuberculosis, tubo-ovarian abscess, and trauma.2 Often, the physical examination remains unremarkable and there are no palpable well-defined abdominal or pelvic masses.3
Ultrasound is the most frequently used imaging investigation in the initial workup of abdominopelvic pain. Typically, a peritoneal inclusion cyst is seen as an anechoic fluid collection containing multiple septations, along with a normal ovary. The fluid can be echogenic secondary to hemorrhagic or proteinaceous material. Sometimes, adhesions surround the ovary and fluid accumulates forming a cystic mass. The trapped ovary has the appearance of what has been described as a “spider in a web”.4 Sonographic features, however, are non-specific. CT scans similarly give a cobweb appearance of loculated fluid with septations within, containing material with the attenuation properties of fluid or hemorrhage. It is critical to be familiar with this benign disease and its clinical and radiological features to make the diagnosis. In cases where USG and CECT findings are equivocal, magnetic resonance imaging (MRI) should be considered for demonstrating the relationship of the cyst to the ovary accurately. On MRI, cystic lesions with low T1 signal and high T2 signal consistent with serous fluid are seen, except in hemorrhage cases when a high T1 signal is demonstrated.5 MRI may also be helpful in defining the extraovarian nature of fluid collection(s).
Management can be both conservative and surgical in patients with a peritoneal inclusion cyst. Asymptomatic patients with incidentally discovered cysts can simply be kept under observation. The use of oral contraceptives is thought to decrease the amount of fluid produced by the ovary and are frequently used for suppressive treatment. Image-guided aspiration, drainage, and sclerotherapy have also been attempted for symptom relief. Multiple large cysts or recurrent peritoneal inclusion cysts are managed with cyst excision, total hysterectomy, and bilateral salpingo-oophorectomy. However, there is a risk of local recurrence irrespective of the procedure undertaken.
references
- 1. Veldhuis WB, Akin O, Goldman D, Mironov S, Mironov O, Soslow RA, et al. Peritoneal inclusion cysts: clinical characteristics and imaging features. Eur Radiol 2013 Apr;23(4):1167-1174.
- 2. Singh A, Sehgal A, Mohan H. Multilocular peritoneal inclusion cyst mimicking an ovarian tumor: A case report. J Midlife Health 2015 Jan-Mar;6(1):39-40.
- 3. Amesse LS, Gibbs P, Hardy J, Jones KR, Pfaff-Amesse T. Peritoneal inclusion cysts in adolescent females: a clinicopathological characterization of four cases. J Pediatr Adolesc Gynecol 2009 Feb;22(1):41-48.
- 4. Savelli L, de Iaco P, Ghi T, Bovicelli L, Rosati F, Cacciatore B. Transvaginal sonographic appearance of peritoneal pseudocysts. Ultrasound Obstet Gynecol 2004 Mar;23(3):284-288.
- 5. Yaegashi N, Yajima A. Multilocular peritoneal inclusion cysts (benign cystic mesothelioma): a case report. J Obstet Gynaecol Res 1996 Apr;22(2):129-132.