In 2015, 36.7 million people globally were estimated to be living with HIV, 2.1 million people were newly infected, and 1.1 million people had died from the disease. Since the start of the epidemic, 78 million people have become infected with HIV, and 35 million people have died from AIDS-related illnesses.1 By the end of 2015 in the Eastern Mediterranean Region, it was estimated that 330 000 people were living with HIV (PLHIV), of those an estimated 75 000 people became infected with HIV. There were 24 000 related deaths in the same year.2
The Omani National AIDS Program (NAP) was established in 1987 and an HIV/AIDS section was established as an integral part of the Department of Communicable Disease Control, Ministry of Health (MOH), in 1990. Since 1996, the NAP has been one of the 12 programs integrated into the National Strategic Planning for the health sectors. In 1984, a National HIV/AIDS Committee was established consisting of concerned stakeholders, and by 2014, the committee was integrated into Communicable Disease National Committee.
The NAP is the apex body responsible for formulating national policies and implementing the program. It aims primarily to control HIV and transmission of sexually transmitted infection (STI) in the community in general and among key populations as well as improve the physical and psychological health and social conditions of PLHIV and their families. It also aims to control morbidity and mortality due to associated opportunistic infections and encourage and support the efforts of non-governmental organizations working to control HIV risk behaviors and support people with HIV and those affected.
Despite a few publications on HIV in Oman,3–5 there is a dearth of published studies describing the epidemiology of HIV in Oman. In this review, we aim to provide a general overview of HIV in Oman including the disease trend and most prevalent areas and describe the populations most-at-risk of HIV transmission, as well as assess the current treatment strategies to prepare for the challenges ahead. We hope this review will provide a novel and comprehensive insight into the state of the epidemic in Oman and the way forward.
We collected HIV/AIDS data from 1984 to 2015 from Annual Health Reports,3 Annual MOH progress reports, Community Health and Diseases Surveillance Newsletters, and national HIV guidelines. These provided information for calculation of the different HIV/AIDS indicators including HIV/AIDS prevalence per 100 000 population, mortality, and case demographics (age, sex, nationality, and residency). A p-value < 0.050 was a cut-off point for the significance of the association with various parametric tests and the Chi-square test.
National political commitment
Political support and leadership are reflected in the readiness expressed by policymakers within the MOH and other stakeholders to support the National HIV and AIDS Strategic Plan (2008–2011 and 2012–2015), as well as adequate allocation of human and financial resources across the country. Oman has a long-existing commitment for free access to testing, counseling, and comprehensive treatment, care, and support for PLHIV.
Disease surveillance
National disease surveillance was established in 1987, and HIV case reporting was integrated into the National Communicable Disease Surveillance System under group A (i.e., diseases that should be notified within 24 hours). Both HIV biological and behavioral surveillance were implemented targeting key populations (i.e., pregnant woman, tuberculosis (TB) cases, intravenous drug users (IDUs), blood donors, prisoners, those with STIs, and renal dialysis candidates). The surveillance monitors prevalence along with other notifiable communicable diseases. Each governorate has an HIV focal point and is responsible for providing relevant details of PLHIV to the NAP.
Case ascertainment and testing
HIV and AIDS are mandatory reportable conditions. Both active and passive HIV surveillance were adopted nationally, maintained and intensified, targeting suspected HIV cases and key populations. The HIV suspected patient is usually screened based on national and World Health Organization (WHO) guidelines.6,7 If confirmed, he/she is referred to the general physician closest to their residential area. The MOH reporting policy requires all health institutions, including non-MOH (private) institutions, to notify suspected and confirmed HIV cases as early as possible to the nearest assigned governorate’s Communicable Diseases Surveillance and Control Unit. Passive surveillance includes reporting of suspected HIV cases by the health care provider and should generate the notification, while active surveillance is done through HIV testing conducted systematically among key targeted populations including prisoners, pregnant women, IDUs, TB cases, close contact individuals (spouse, partners, client), renal dialysis candidates, blood donors, and foreign-born individuals applying for residency.6 All foreign-born workers seeking residency in Oman are mandatorily screened for HIV in their country of origin before they are granted a residence permit. They are also retested on renewal of their contracts.
Children (≤ 18 months old) born to mothers with an unknown HIV status or a HIV-positive mother follow a separate diagnostic algorithm. HIV polymerase chain reaction test (viral load) is used for diagnosis in children < 18 months old.6
Samples are tested using the WHO recom-mendations and national guidelines.6,7 All testing is carried out in the public health laboratories at governorate levels. One public health laboratory is dedicated at each governorate for ELISA HIV testing. The national laboratories participated in the internal quality assurance program conducted by the United Kingdom National External Quality Assessment services.
Initiation of voluntary counseling and testing (VCT) service providers in 2013 and anonymous testing among most-at-risk populations (MARPs) in 2007 were a major step towards early diagnosis. Anonymous testing among MARPs was established in 2007 in three governorates (Muscat, Sohar, and Al Buraimi).
HIV counseling
Voluntary counseling is offered to both nationals and foreign-born residents, including pre-test counseling covering the health implications of HIV and post-test counseling services after test results are ready.6
Verbal consent is obtained before collection of the sample for HIV testing. The client should voluntarily agree to have his/her blood tested for HIV. This consent should be based on sufficient, accurate, and clear information. The minimum package of information for an informed consent will cover the following main points: reasons why HIV testing is recommended, details, risks, and implications of HIV testing and the meaning of test results; the post-test follow-up prevention and treatment services available, when needed; assurance of confidentiality; and disclosure strategy and any further inquiries by the patient.
HIV counselors are available in most primary, secondary, and tertiary care centers. They are equipped with the required skills to perform contact management, to preserve confidentiality and ensure long-term compliance for HIV treatment and care.6
Treatment and care
The program adopts a management policy of giving antiretroviral therapy (ART) regimens as recommended by the WHO for all HIV cases.6 Patients are managed and followed-up at polyclinics, and secondary and tertiary care hospitals. Diagnosed cases will be linked to HIV treatment centers for lifelong treatment and care. Antiretroviral drugs are made accessible to all the governorate tertiary and secondary hospitals and polyclinics.
Contact tracing and follow-up
Sexual contacts of any HIV-positive cases including spouse or partner and all children delivered by HIV-positive woman and needle-sharing partners are screened and counseled for HIV. However, a follow-up program to teach behavior change is needed.
HIV monitoring system
The governorate Communicable Diseases Surveillance Unit collects and compiles monthly summaries from specialized clinics of both public and non-public providers. These include the number of total positive HIV cases, residence, sex, age, nationality, sexual contacts details, stage of treatment, and relapse. Monitoring also includes adherence, treatment failure, severe reactions, and complications and possible toxicities of ART. Such data are disaggregated from subunits to the central level monthly.
Epidemiology of HIV
In 1984, the first AIDS case was reported in Oman. The number of cases significantly and steadily increased to 1994. When comparing the decades 1984–1995 and 1996–2015 more than 80.0% of the cases were reported in the latter decade [Figure 1]. Thereafter, annually, an average of about 250 cases were reported with an average of 148 new cases among nationals and 100–200 cases among foreign-born residents. As of 2015, there are approximately 2879 PLHIV. Of those, 1945 (67.6%) know their HIV status.
We observed a mild decreasing trend in HIV cases among Omanis from 143 to 142 and a rising trend (60.0%) in foreign-born citizens from 129 to 214 from 2010 to 2015. In the past 30 years (1984–2015) Oman has had a total of 2622 HIV-positive cases giving a national prevalence of 1.0% [Figure 1].
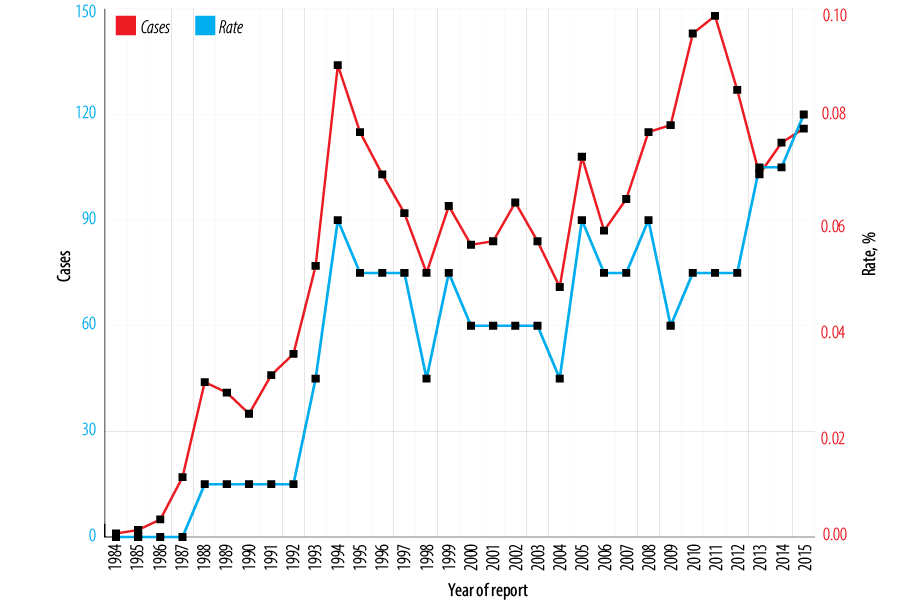
Figure 1: HIV cases and rates in Oman from 1984 to 2015.
Gender and age group
Of the total HIV cases, males (n = 1896) were affected more than females (n = 726) (p < 0.001); 1322 (69.7%) of affected males and 531 (73.1%) females were aged 20–49 years and 19 (1.0%) males and 14 (1.9%) females were adolescents aged 10–19 years. Sixteen (0.8%) males and 10 (1.4%) females were children aged 0–9 years. Five-hundred and ten (26.9%) males and 110 (15.2%) females were aged > 50. The distribution of HIV had an upward trend among males across all age groups with the least cases reported among those aged < 15 years old. The number of new detected cases every five years followed an upward trend [Figure 2].
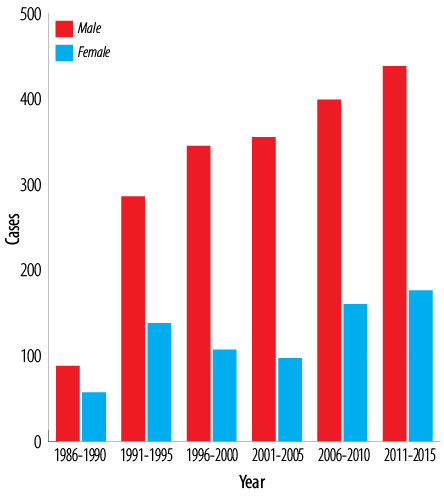
Figure 2: Cases of HIV in Oman by gender, five-year intervals trend (1986–2015).
Geographical distribution
The governorate of Buraimi was the most severely affected geographical area (617/100 000 population) followed by Musandam (267/100 000 population) and North Sharqiyah (239/100 000 population) [Figure 3].
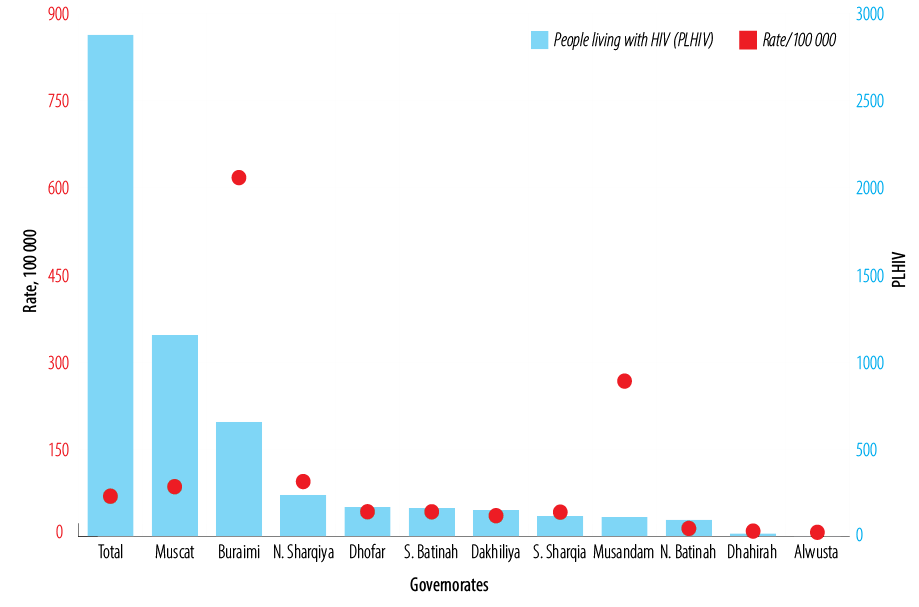
Figure 3: HIV cases and rate/100 000 population by governorate in 2015.
Mode of transmission and MARPs
The main mode of HIV transmission was through sex (n = 1751, 66.8%), of which heterosexuals and bisexuals, and men who have sex with men (MSM) were 1017 (38.8%) and 734 (28.0%) of cases, respectively. Mother-to-child transmission (MTCT) were 218 (8.3%) cases, intravenous drug abuse was 112 (4.3%), blood transfusion was 84 (3.2%), and unknown causes were 457 (17.4%) of all cases [Table 1]. Since 1995, transmission of HIV by blood has not been reported. The prevalence of HIV among patients with TB has ranged between 2–4%. The prevalence of HIV in prisoners was 0.4% in 2007, 0.8% in 2009, 0.3% in 2010 and 2011, 0.5% in 2012, and 0.8% in 2013. In patients with STI, the prevalence of HIV was 0.4% in 2007, 2.3% in 2008 and 2009, 0.2% in 2010, 0.02% in 2011, 0.04% in 2012, and 0.007% in 2013. The prevalence of syphilis among pregnant women was 0.2% in 2007, 0.1% in 2008, and 0.05% in 2011 and 2013. As reported, more than 99.0% of pregnant women are tested for HIV and syphilis.
Table 1: Route of HIV transmission in Oman, 1982–2015.
|
Sexual |
1751 (66.8) |
|
Heterosexual |
1017 (38.8) |
|
Bisexual and men who have sex with men |
734 (28.0) |
|
Mother-to-child |
218 (8.3) |
|
Blood transfusion |
84 (3.2)* |
|
Intravenous drug abuse |
112 (4.3) |
|
Unknown |
457 (17.4) |
*the last cases of HIV due to blood donor reported in 1995.
a) Intravenous drug use
A Rapid Situation Assessment of HIV risks among IDU in Muscat was carried out in December 2006 (unpublished). It was a qualitative and quantitative survey carried out among heroin, cocaine, or injecting drug users. The qualitative section consisted of in-depth interviews of key informants (n = 6), drug users (n = 22), and one focus group. The quantitative part of the survey included three separate samples: community-based drug users (n = 132), prison-based drug users (n = 34), and treatment center-based drug users (n = 18).
The results revealed that the majority of participants reported to have shared equipment (90% of the community-based group, 97% of the prison-based group, and 94% of the treatment center-based group). Some had even used equipment that had been used by a person they knew to be HIV-positive (23% of the community-based group, 24% of the prison-based group, and 39% of the treatment center-based sample). A sub-sample of IDUs were tested for HIV, the seroprevalence reported by those previously tested was high; 18% (n = 97) in community-based participants, 27% (n = 33) in prison-based participants, and 12% (n = 17) in treatment center-based participants. All tested HIV-positive participants knew their HIV status before the study.
Data from the National Narcotics and Psychoactive Registry suggested a concentrated epidemic among drug users. The HIV seroprevalence among IDUs admitted in treatment centers was about 23% in 2004, 15% in 2005, and 8% in 2006.8 HIV seroprevalence among IDUs seemed to decline between 2013 and 2015.8 However, the majority of injecting drug user population was of unknown status in 2015 due to not taking part in the testing process. This implies the need for a call to action, especially regarding bias and stigma associated with testing and treating injecting drug users. The key risk behavior that exposes people who inject drugs to HIV infection is the use of non-sterile injecting equipment. Available data indicate that the majority of this group will ultimately use non-sterile injecting equipment giving a lifetime prevalence of sharing needles and syringes of 97%.9
b) Prevention of mother-to-child transmission
From July 2009, Oman initiated HIV testing and counseling services to all pregnant women with the objective of early detection of HIV among pregnant women, provision of care and support to HIV-positive women, and prevention of HIV transmission from women to their infants. During the screening period, the annual average percentage of HIV testing was 98%. Of the total pregnant woman screened, 90 HIV-positive cases were identified suggesting a cumulative HIV seroprevalence among pregnant women of 0.02%. The annual distribution of the cases was five in 2009 (July–December), 21 in 2010, 16 in 2011, 17 in 2012, 22 in 2013, and nine in 2014 (p < 0.001). There were 31 HIV-positive infants born to HIV-positive mothers. The percentages of MTCT of HIV were 60%, 23%, 63%, 35%, 18%, and 33% in 2010, 2011, 2012, 2013, and 2014, and 2015, respectively (p < 0.001). No information was collected on breastfeeding/non-breastfeeding rates among HIV-positive infants born to HIV-positive mothers. The rates of infection due to MTCT per 100 000 live births were 11, 9, 17, 10, 6, and 4 from 2009 to 2014, respectively.10
HIV management and care
HIV-positive patients are treated at 15 different sites all over Oman. Of these, Muscat governorate has the highest number of patients seeking treatment. From mid-2007, the MOH advised, in accordance with WHO recommendations, that patients with a CD4 count < 500 be giving ART, and as of 2016 a ‘treat all’ policy was adopted.
In six years (2010–2015), the number of cases on ART increased by 57.0% from 469 to 1098 p < 0.0001). By 2015, ART coverage was 65.0%, varied by governorate from 50% and 91%, with highest coverage reported from Musandam and Al Wusta governorates.
There were 632 new HIV infected cases diagnosed between 2011 and 2016. Although all patients had their CD4 cell count taken at the time of diagnosis, there was a delay in diagnosis of 272 days noted among 327 (51.7%) cases. Of the cases diagnosed without any delay, 305 (48%) achieved viral suppression.
Average HIV-related mortality between 2002–2005, 2006–2010, and 2011–2015 was 30, 31, and 23 cases, respectively, with 23.0% reduction in the two latter periods noted (p < 0.0001).
Program success, challenges, and remedial actions
There have been important achievements and successes in Oman. Best practices include adopting a comprehensive national response HIV strategic plan, free access to comprehensive treatment, care for PLHIV, and good laboratory support and well-trained staff. Blood transfusion services provide safe and effective services, and HIV transmission through blood or blood products can virtually be ruled out. HIV patients are protected in general legally through policies for employment and human rights. The wide availability of ART across the country might be an attributing factor to the declining rate of HIV-related mortality.
Since 2009, the near-universal access to antenatal screening has minimized HIV transmission from mother-to-child and consistently achieved > 90% coverage. However, the program needs to continue maintaining and achieving high coverage of ART treatment and chemoprophylaxis for HIV-positive mothers and intensive efforts to eliminate MTCT of HIV to ensure a further reduction in HIV infections among infants born to HIV-positive mothers to zero.
Initiation of anonymous testing among MARPs and VCT is a major step towards early diagnosis and implementation are encouraging. Additionally, the Omani NAP is planning to expand it to more areas in the near future.
Efforts have also focused on improving HIV estimations as well as improving the quality and usability of routine case report data to understand the need for HIV prevention and treatment better.
Another key achievement was the increasing collaboration between the NAP and civil society organizations especially for studies of IDU. They reflect the acknowledgment that partnerships which build on the comparative advantages of governmental, civil societial, and private sectors can create win-win situations.
HIV awareness of the general population has taken place mainly around World AIDS Day and festivals. There have been ongoing efforts in the field of HIV education and peer outreach for young people and youth outreach activities, which draw large groups of young people. These efforts have so far taken place on a modest and ad-hoc basis, reaching relatively small numbers of youth making the impact of these one-off interventions limited. Another good opportunity to raise HIV awareness are during screening campaign activities (e.g., for blood donors; foreign-born; antenatal clinic clients; TB and STI patients; pre-marital screening; patients admitted to hospitals for invasive procedures and organ transplants; prisons and those arrested by the police), which reach large groups of people, but are currently not accompanied by HIV education messages. Furthermore, there have been ongoing efforts in the field of HIV education and peer outreach for young people and youth outreach activities, the lessons learned can be used to develop more effective HIV education approaches for young people, including out-of-school youth. While HIV education has been part of the curriculum for school children for a long time, sensitive issues surrounding sexuality and relationships, and school-based education mainly focused on medical facts. Other challenges remain, given the taboos and sensitivities surrounding sex education for children and young people. The Peer Education Program on HIV for young people is another joint effort between the MOH and Ministry of Education in the field of peer education for young people on HIV, which needs further strengthening.
Oman is facing rapid changes in sexual behavior patterns among young generations, especially among young men, highlighting the importance of conducting comprehensive research to identify the scale and scope of risk behaviors among Omani youth and develop appropriate HIV prevention programs. A hotline, managed by volunteers, was initiated to answer any concerns with HIV.
The major challenge facing the NAP is non-adherence and poor compliance to ART due to various reasons, such as a lack of resources to travel to the ART facility on a regular basis which leads to loss of follow-up with some patients. Other treatment problems are related to the late diagnosis of HIV cases, which lead to premature death. Henceforth, contributing barriers need to be identified and managed. Other challenges with regard to treatment access is the fact that stigma and discrimination exist among health care workers and patients.
An important challenge is related to the fact that HIV prevalence in the general population has remained < 1%,1 and was considerably higher among IDU populations.9 In addition, there was much variation among deferent governorates with the highest rates in Al Buraimi. Since the HIV epidemic is concentrated among IDU populations, HIV has never been identified as a priority public health problem. As a result, sustained political support remains a challenge. In this context, it is difficult to ensure a systematic and sustained HIV response. Therefore, strong evidence and effective advocacy are required to convince high-level decision-makers of the need to further strengthen HIV prevention.
Oman has taken several steps towards promoting substance misuse harm reduction among IDU, with an overall objective of controlling HIV and other blood-borne infections.
HIV surveillance of high-risk groups including IDU, MSM, and sex workers (as recommended by the WHO for countries with low and concentrated HIV epidemics) is to be established in the country. Further, institutional strengthening is needed for the effective functioning of the national Monitoring and Evaluation Committee as the key multi-sectorial coordination body.
The HIV epidemic, and the existence and scale of high-risk behaviors and effective interventions makes it difficult to establish an effective HIV prevention program. The absence of adequate biological and behavioral surveillance systems and effective monitoring and evaluation systems hampers an evidence-informed approach, which comprises of effective national policies and strategic frameworks, as well as adequate budgets. The suggested remedial actions include: 1) Research into the social and behavioral dynamics of MARPs, as well as youth and other vulnerable groups that increase HIV risk; 2) Strengthening of existing surveillance systems, and establishment biobehavioral surveillance studies among MARPs; as well as improved national monitoring and evaluation systems that support effective information flows from data collection down to the use of data for evidence-informed decision-making; 3) Operational research that allow assessing and identifying effective HIV interventions based on the specific service needs of PLHIV and MARP is paramount as there is limited research among the most-at-risk populations, including sex workers, MSM, and IDU, and the available data and information from key informants show that these MARP are all present in Oman and face considerable HIV risks. These groups may contribute to the further spread of HIV, not only among MARP groups themselves.
Progress towards the 90–90–90 target adopted by United Nations General Assembly by 202011 (the aim was to diagnose 90% of all HIV-positive persons, provide ART for 90% of those diagnosed, and achieve viral suppression for 90% of those treated) and intensive focus on five prevention pillars delivered through a people-centered, combination approach. In 2015, there were an estimated 67.6% of PLHIV; about 65.0% were on ART nationally and only 48.0% of those on treatment were achieving virological suppression. There are considerable gaps to reach the 90–90–90 target in Oman, and there is a need to identify and manage barriers.
Conclusions
While the prevalence of HIV infection in Oman continues to be < 1%,1 the NAP needs to focus on key areas including quality and coverage of treatment, care and support (with special attention for MARP groups), foreign-born, and the expansion of anonymous testing and VCT services. There is also a need to step up public awareness of the disease especially among youth along with a series of multiple preventive services including peer education for young people. There is an urgent need to address existing gaps in understanding of HIV transmission and establish testing and treatment within IDU, MSM, and sex worker populations based on WHO guidelines.12 Finally, to achieve the 90–90–90 target, Oman should identify and manage any contributing barriers.
Disclosure
The authors declared no conflict of interest. No funding was received for this study.
Acknowledgements
We are indebted to H.E. Dr. Ali Bin Moosa, late H.E. Dr. Ali Jaffer Mohammed, late H.E. Dr. Ahmed Al Ghassani, H.E. Dr. Mohammed Al Hosani, late Dr. Rauf Al Suwedi, Dr. Ali Baomar, Dr. Mohammed Ridha, Dr. Suleiman Al Busaidi, Dr. Said Al Baqlani, Dr. Mohammed Faraj, Dr. Tareq Baha, Dr. Aleksandra Caric, Dr. Adamu, all governorate epidemiologists and counselors, treating physicians and Miss Magda Salim Al Wahebi, for their vision and guidance.
references
- 1. AIDS by the numbers. UNAIDS. 2016 [cited 2017 December]. Available from: http://www.unaids.org/sites/default/files/media_asset/AIDS-by-the-numbers-2016_en.pdf.
- 2. Global report: UNAIDS report on the global AIDS epidemic 2015. UNAIDS/10.11E/JC1958E). [cited 2017 December]. Available from: www.unaids.org/en/resources/documents/2015/AIDS_by_the_numbers_2015.
- 3. Annual Health Report, 2005-2015, Ministry of Health, Oman. [cited 2017 December]. Available from: www.moh.gov.om/en/web/statistics/annual-reports.
- 4. Scrimgeour EM, Mehta FR, Suleiman AJ. Infectious and tropical diseases in Oman: a review. Am J Trop Med Hyg 1999 Dec;61(6):920-925.
- 5. Gökengin D, Doroudi F, Tohme J, Collins B, Madani N. HIV/AIDS: trends in the Middle East and North Africa region. Int J Infect Dis 2016 Mar;44:66-73.
- 6. Management HI. in Oman. A guide for health care workers, 3rd ed. 2015. [cited 2017 December]. Available from: www.moh.gov.om/en/web/directorate-general-of-disease-surveillance-control/resources.
- 7. WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related diseases in adult and children. [cited 2017 December]. Available from: http://www.who.int/hiv/pub/guidelines/HIVstaging150307.pdf?ua=1.
- 8. Statistics of the national registry for addiction, MOH, 2004-2015. [cited 2017 December]. Available from: www.moh.gov.om.
- 9. Mumtaz GR, Weiss HA, Thomas SL, Riome S, Setayesh H, Riedner G, et al. HIV among people who inject drugs in the Middle East and North Africa: systematic review and data synthesis. PLoS Med 2014 Jun;11(6):e1001663.
- 10. Jaffer YA, Al-Awaidy ST. Elimination of mother-to-child transmission of HIV, an experience from Oman. J HIV AIDS 2017;3(1).
- 11. Prevention gap report, HIV UNAIDS. 2016 [cited 2017 December]. Available from: www.unaids.org/en/resources/documents/2016/prevention-gap.
- 12. Global HIV Strategic Information Working Group. Bio-behavioral survey guidelines for populations at risk for HIV. [cited 2017 December]. Available from: http://who.int/iris/bitstream/10665/258924/1/9789241513012-eng.pdf?ua=1.