The internship period for medical doctors has been variously described as a “rite of passage endured between graduation and early working life, a stress test before practice”.1 During the year, interns are responsible for patient care, learning new skills, and assisting in procedures of which they have no prior experience. The concept of residents’ perceptions of their own preparedness for clinical work has been explored in many research studies from western countries, with some studies comparing levels of preparedness between graduates from different teaching models.2−4
Globally, many researchers highlighted the gap between the undergraduate medical education,
which prepares medical students for hospital practice and what hospital work really requires. Several previous studies have focused on interns’ self-assessment of their skills.5−8 Other studies have concentrated on the views of the supervisors, the clinical teams, or service users.9−11 There were also comparisons and contrasts of different preparation for practice curriculums by different medical schools.12,13
A number of studies focused on the contribution of pre-internship training towards preparing senior medical students for workplace practice.7,8,14 One study looked at the impact of the internship training site itself on the junior doctors’ perceived preparedness.15 With regards to methodology, previous studies in this field utilized questionnaires, semi-structured interviews, and focus group discussions to address the preparedness for practice. Concerning the Middle East, there is a dearth of studies exploring this concept. In Germany, a study showed 60% of the participants reported deficiency in practical skills such as electrocardiogram (ECG) interpretation, planning treatment, and intubation. While in a study from Kenya, both interns and their clinical supervisor were interviewed and reported that interns lacked preparedness in performing practical skills, managing clinical challenges, and communication skills.14
A study by Kassim et al,15 compared perceptions of preparedness for hospital practice between graduates from medical schools in Dublin, Ireland, and Bahrain. It showed that graduates from Bahrain scored higher in the domains of confidence, holistic care, and self-directed learning than the Irish graduates who felt more prepared for interpersonal relationships with patients.15
The Oman Medical Specialty Board (OMSB) was established in Oman in 2006 to oversee the postgraduate medical education and training.16 There are currently 18 specialty postgraduate programs registered under OMSB, and many of these have applied to be accredited by the Accreditation Council for Graduate Medical Education’s-International (ACGME-I), the international arm of ACGME.17
Residents who enroll in the postgraduate medical training are mostly graduates from Sultan Qaboos University (SQU), Oman Medical College (OMC), a private medical college in Oman,
and a small number of graduates come from overseas medical schools, such as the University of Auckland. Graduates from the three aforementioned universities undergo an approved internship training in Oman under the direct supervision of the College of Medicine and Health Sciences (CoMHS) at SQU to ensure the quality and equal distribution of interns to different hospitals in Oman, which in turn leads to the smooth running of the program.18 The number of years spent in undergraduate medical training is almost the same in the three mentioned universities. However, there are a few variations in the content of each year. For example, undergraduates at the University of Auckland get introduced to the fundamentals of clinical practice during their second year of medical school,19 while SQU and OMC graduates have their clinical placements from third year onwards.20,21
Studies related to the perception of preparedness of junior doctors in Oman are limited. To the best of our knowledge, this is the first study exploring the perception of preparedness among junior medical doctors from Oman. The current study had two aims. First, to evaluate the new residents’ overall perceptions of preparedness for clinical practice, measured by the Preparation for Hospital Practice Questionnaire (PHPQ). Second, to correlate between the mean rank scores of the PHPQ’s eight domains and the residents’ demographics (age, gender, place of undergraduate study, and length of internship).
Methods
This cross-sectional study was conducted at OMSB between 20−23 August 2016. The study was approved by the OMSB Research Ethics Committee. Participants were informed that they could withdraw from the study at any point.
The study population were new graduates from CoMHS at SQU, OMC, and the University of Auckland School of Medicine who were accepted as new residents in various specialty training programs of OMSB.
In this cohort, all 160 newly accepted residents attending a mandatory induction workshop were invited to participate. Residents who did not sign the informed consent forms or provided incomplete questionnaires were excluded.
The new residents’ preparedness was assessed using the PHPQ. This is a previously validated and reliable 41-item self-rated questionnaire, which contains eight subscales designed to assess key areas of medical hospital practice as outlined below:21
- Interpersonal skills (effective and competent communication with patients).
- Confidence and coping.
- Collaboration (team approach to care).
- Patient management and practical skills.
- Understanding science (as the basis of disease and therapeutics).
- Prevention (preparedness to incorporate health promotion and disease prevention with hospital practice).
- Holistic care (appreciation of the impact of multiple variables on patients’ health and disease).
- Self-directed learning (evaluation of performance and identification of learning needs).
Participants were asked to rate their responses on a five-point Likert Scale (1 = not prepared to 5 = fully prepared) in response to statements like: “My medical training prepared me to...”. The PHPQ subscales’ reliability alpha coefficients ranged from 0.78−0.88 as stated in a study by Hill et al.21 Information regarding the residents’ age, gender, their undergraduate medical school, year of graduation, length of post-internship role as general practitioner (GP), posting, and specialty were also collected.
Data were described using frequency, percentage, and mean scores. The overall mean rank score of the PHPQ was classified into “well prepared” (score 3.5−5), “fairly well prepared” (2.5−3.4) and “less than adequately prepared” (1.0−2.4). Associations between the participants’ characteristics and their level of preparedness mean ranks were evaluated using chi-square, Mann-Whitney U, and Kruskal-Wallis H tests of association. Dunn’s post hoc multiple comparison tests were performed following a statistically significant Kruskal-Wallis test. A two-tailed level of significance was set at p = 0.050. The study power (1-b) was 80%. All the statistical analysis was carried out using SPSS Statistic (IBM Corp. Released 2013, IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.) version 22.
Results
The response rate of the study was 87.5%. Among the 140 participants who responded, 70.7% were female and 59.3% graduated from SQU [Table 1]. As shown in Figure 1, 99.0% of the graduates were either “well prepared” or “fairly well prepared” for hospital practice.
Table 1: Socio-demographic characteristics of the participants.
|
Gender |
|
|
Male |
41 (29.3) |
|
Female |
99 (70.7) |
|
Age, years |
|
|
≤ 26 |
69 (49.3) |
|
> 26 |
71 (50.7) |
|
Specialty |
|
|
Anesthesia |
10 (7.1) |
|
Biochemistry |
4 (2.9) |
|
Dermatology |
5 (3.6) |
|
ENT |
7 (5.0) |
|
Emergency Medicine |
8 (5.7) |
|
Family Medicine |
17 (12.1) |
|
Hematology |
4 (2.9) |
|
Histopathology |
2 (1.4) |
|
Internal Medicine |
17 (12.1) |
|
Microbiology |
4 (2.9) |
|
OBGYN |
9 (6.4) |
|
OMFS |
2 (1.4) |
|
Ophthalmology |
4 (2.9) |
|
Orthopedics |
4 (2.9) |
|
Pediatrics |
22 (15.7) |
|
Psychiatry |
5 (3.6) |
|
Radiology |
6 (4.3) |
|
Surgery |
10 (7.1) |
|
Medical school |
|
|
Sultan Qaboos University |
83 (59.3) |
|
Oman Medical College |
43 (30.7) |
|
University of Auckland |
14 (10.0) |
|
Year of graduation |
|
|
2009-2014 |
67 (47.9) |
|
2015 |
73 (52.1) |
|
Post-internship GP placement |
|
|
Yes |
|
|
≤ 1 year |
32 (22.9) |
|
> 1 year |
31 (22.1) |
ENT: ear, nose and throat; OBGYN: obstetrics and gynecology; OMFS: oral and maxillofacial surgery; GP: general practitioner.
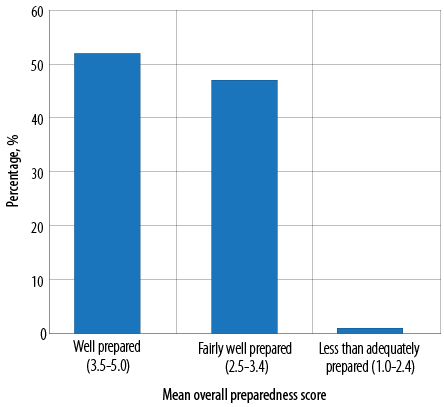
Figure 1: Mean overall preparedness score of all participants.
Mean ranks for the domains of the PHPQ were shown in Table 2. There was no statistically significant association between the domains and the participants’ age. Male participants scored significantly higher in the management domains compared to the female participants (Mann-Whitney U = 1539.000; p = 0.024).
Table 2: Comparison between PHPQ domains and different characteristics of participants.
|
Gender |
|
Male |
76.80 |
64.41 |
71.43 |
82.46 |
76.87 |
73.46 |
71.91 |
71.15 |
|
Female |
67.89 |
73.02 |
70.12 |
65.55 |
67.86 |
69.27 |
69.91 |
70.23 |
|
p-value+ |
0.234 |
0.252 |
0.861 |
0.024* |
0.228 |
0.576 |
0.790 |
0.903 |
|
Age, years |
|
≤ 26 |
64.25 |
68.59 |
72.83 |
69.01 |
71.72 |
71.78 |
72.16 |
72.19 |
|
> 26 |
76.57 |
72.35 |
68.23 |
71.95 |
69.31 |
69.26 |
68.89 |
68.86 |
|
p-value+ |
0.071 |
0.582 |
0.499 |
0.666 |
0.722 |
0.712 |
0.632 |
0.625 |
|
Place of graduation |
|
SQU |
61.80 |
58.93 |
66.43 |
71.80 |
66.13 |
61.68 |
63.94 |
65.66 |
|
OMC |
78.98 |
83.59 |
69.98 |
64.73 |
72.65 |
80.07 |
74.14 |
72.86 |
|
Auckland |
84.36 |
87.95 |
84.55 |
64.59 |
76.41 |
80.95 |
87.09 |
79.14 |
|
p-value++ |
0.028* |
0.001* |
0.352 |
0.589 |
0.547 |
0.027* |
0.111 |
0.420 |
|
Duration of internship |
|
≤ 1 year |
28.41 |
32.55 |
32.86 |
29.89 |
26.45 |
31.72 |
32.61 |
29.75 |
|
> 1 year |
35.71 |
31.44 |
31.11 |
34.18 |
37.73 |
32.29 |
31.37 |
34.32 |
**All results are shown as mean rank. PHPQ: preparation for hospital practice questionnaire; SQU: Sultan Qaboos University; OMC: Oman Medical College.
*Statistically significant (p < 0.050); +Mann-Whitney U test; ++Kruskal-Wallis H test.
Duration of post-internship GP placement had a statistically significant association with the “understanding science” domain. Graduates who did more than one year of post-internship GP placement scored higher in the “understanding science” domain (Mann-Whitney U = 318.500; p = 0.013) compared to those who did less than or equal to one year.
There were statistically significant differences in the domain scores of “interpersonal skills” (Kruskal-Wallis H, c2 (2) = 7.183; p = 0.028), “confidence” (Kruskal-Wallis H, c2 (2) = 13.760; p = 0.001) and “prevention” (Kruskal-Wallis H, c2 (2) = 7.237; p = 0.027) between the participants from different medical schools (SQU, OMC, and the University of Auckland). Subsequently, pairwise comparisons were performed using Dunn’s (1964) procedure with a Bonferroni correction for multiple comparisons. This post hoc analysis revealed a statistically significant difference in the domain score of “confidence” between SQU (mean rank = 58.93) and OMC (mean rank = 83.59) (p = 0.003). It also revealed a statistically significant difference in the domain score of “prevention” between SQU (mean rank = 61.68) and OMC (mean rank = 80.07)(p = 0.040). However, there was no statistically significant difference in the domain score of “interpersonal skills” between these groups based on post hoc analysis.
Discussion
According to the overall score, the results indicated that most of the residents were either “well prepared” or “fairly well prepared”, with scores of 52% and 47%, respectively. Similar results were reported in a study from Stellenbosch University in South Africa where participants reported feeling well prepared for most mainstream clinical activities.22 Another study by Chen et al, 23 in the United States, reported that 53.8 % of the 2 287 residents felt very well or mostly prepared with regards to their medical knowledge and clinical skills. This congruence of overall preparedness score with international studies’ scores could be explained by the fact that most of the participants in our study were the best candidates chosen by the board selection committees to be enrolled in the 18 specialty training programs at OMSB. In addition, the overall preparedness was assessed by averaging the scores of all eight domains of PHPQ, however, noticeable differences were reported between the residents in some areas of perceived preparedness. For instance, the findings from this study demonstrated a variation between graduates from the three medical schools, with graduates from OMC perceiving themselves to be more confident than SQU graduates. This can be explained by the variation in the curricula in different medical schools. In accord with our findings, several overseas studies have consistently highlighted the impact of differences in the curricula on young doctor’s self-assessed preparedness and skills. A study of the graduates from the University of Sydney, which teaches a problem-based medical program, perceived themselves to be more prepared in interpersonal skills, confidence, collaboration, holistic care, and self-directed learning compared to graduates from traditional courses.24
A study from New South Wales in Australia found that graduates from a new outcomes-based integrated program cohort felt significantly better prepared for hospital practice than those who graduated from the older medical program, both before and after attending a preparation for internship course focusing on confidence, collaboration, interpersonal skills, and prevention. They also reported significant improvements in the post-course ratings in 3 out of 4 sub-scales (confidence, collaboration, and interpersonal skills) (p > 0.050) compared to graduates of the old medical program.25 Likewise, another study on the perception of preparedness among graduates from three UK medical schools using different curricula (systems-based, integrated curriculum, graduate entry, and problem-based learning), concluded that participants felt well prepared for basic clinical tasks, including history taking, and were confident in their communication skills. However, they felt less prepared in skills such as managing acutely ill patients, prescribing medications, managing their workload, and performing a practical procedure, such as inserting a nasogastric tube.26 Hence, the importance of problem based and integrated medical teaching and training curriculum cannot be overemphasized.
The participants’ age had no impact on their perception of preparedness when analyzed by individual domains. However, previous research has suggested that younger residents were rated better by their supervisors than their older colleagues, particularly in interactional skills.27 This finding could be explained by the absence of any significance variation in the age of the participants in our study.
With reference to gender, this study found that male residents perceived themselves to have better patient management and technical skills. This finding is congruent with some international studies where male residents felt more confident in performing practical procedures.27 This could be due to the fact that male students tend to perform more practical procedures than female students. While Day et al,19 reported in their study that women had more “humanistic” traits than men, others studies reported no correlation between gender and the resident’s level of preparedness to perform technical skills.26
The present study showed the importance of time spent in post-internship GP setting on the scientific knowledge acquired by the participants. Those who spent more than one year in general practice after internship obtained higher score in the science’s domain. This result resonated with international studies reporting similar finding.28,29 One of those studies was a self-assessment and qualitative study of general medical interns, which reported that with regard to post-internship, GP placement appeared to increase the understanding of the basis of diseases and their pharmacological treatment.28 They also reported being better prepared at week 10 of their rotation compared to the first week.28 This finding could be explained by the fact that during their GP work, young doctors (in Oman and other countries) have more exposure to a variety of clinical situations, which they have to make decisions related to treatment options under the supervision of senior colleagues. Also, they have more opportunity to attend workshops and other continuous medical education activities that enhances their understanding on various disorders and their pharmacological intervention.
Although this study did not examine the role of internal factors such as the graduate’s personality, learning style, and external factors like undergraduate clinical placements, shadowing senior colleagues, induction programs, and the support of family and work colleagues, these factors were recognized by other researchers as important correlates of the resident’s perception of preparedness for clinical work.26
Two potential limitations of this study have been identified. Firstly, the self-reporting nature of the data and the use of a rating scale as the outcome measure may have led to inaccuracies related to the validity and reliability of the scale. It is well known that using rating scales may yield a global rating ‘halo’ effect and social desirability, whereby interns’ general perceptions may have influenced their rating of individual questions and areas.30 Secondly, the data collection did not include objective tools such as the residents portfolio or feedback from their clinical tutors. However, despite these limitations, there were some interesting observations which arisen from this study.
Conclusion
The transition that junior doctors make from being students to clinical practice is a period of uncertainty for some, as their perception of their preparedness comes to question. This is an essential stage in the career of junior doctors. Therefore, exploring the factors that influence doctors perception on their preparedness and restructuring the undergraduate curriculum to include more structured evidence based patient contact will boast junior doctors’ confidence in their early clinical years. Such changes will require retraining faculty members and the introduction of work-based assessments at an early stage of the curriculum to evaluate students and provides them with feedback addressing their areas of deficiencies.
Disclosure
The authors declared no conflicts of interest. No funding was received for this work.
Acknowledgements
The authors would like to thank all the residents who participated in this study.
references
- 1. Sasnett B, Ross T. Maximizing internship value by comparing student satisfaction and program competencies. J Community Med Health 2016 Jan;6(1):390-396.
- 2. Millan LP, Semer B, Rodrigues JM, Gianini RJ. Traditional learning and problem-based learning: self-perception of preparedness for internship. Rev Assoc Med Bras (1992) 2012 Sep-Oct;58(5):594-599.
- 3. Brennan N, Corrigan O, Allard J, Archer J, Barnes R, Bleakley A, et al. The transition from medical student to junior doctor: today’s experiences of Tomorrow’s Doctors. Med Educ 2010 May;44(5):449-458.
- 4. Goldacre MJ, Lambert TW, Svirko E. Foundation doctors’ views on whether their medical school prepared them well for work: UK graduates of 2008 and 2009. Postgrad Med J 2014 Feb;90(1060):63-68.
- 5. Cave J, Goldacre M, Lambert T, Woolf K, Jones A, Dacre J. Newly qualified doctors’ views about whether their medical school had trained them well: questionnaire surveys. BMC Med Educ 2007 Oct;7:38.
- 6. Tallentire VR, Smith SE, Wylde K, Cameron HS. Are medical graduates ready to face the challenges of Foundation training? Postgrad Med J 2011 Sep;87(1031):590-595.
- 7. Ochsmann EB, Zier U, Drexler H, Schmid K. Well prepared for work? Junior doctors’ self-assessment after medical education. BMC Med Educ 2011 Nov;11:99.
- 8. Scheffer C, Edelhäuser F, Tauschel D, Riechmann M, Tekian A. Can final year medical students significantly contribute to patient care? A pilot study about the perception of patients and clinical staff. Med Teach 2010;32(7):552-557.
- 9. Matheson C, Matheson D. How well prepared are medical students for their first year as doctors? The views of consultants and specialist registrars in two teaching hospitals. Postgrad Med J 2009 Nov;85(1009):582-589.
- 10. Wall D, Bolshaw A, Carolan J. From undergraduate medical education to pre-registration house officer year: how prepared are students? Med Teach 2006 Aug;28(5):435-439.
- 11. Koh GC, Khoo HE, Wong ML, Koh D. The effects of problem-based learning during medical school on physician competency: a systematic review. CMAJ 2008 Jan;178(1):34-41.
- 12. Bleakley A, Brennan N. Does undergraduate curriculum design make a difference to readiness to practice as a junior doctor? Med Teach 2011;33(6):459-467.
- 13. Jahan F, Siddiqui MA, Al Zadjali NM, Qasim R. Recognition of core elements of medical professionalism among medical students and faculty members. Oman Med J 2016 May;31(3):196-204.
- 14. Maisonneuve JJ, Lambert TW, Goldacre MJ. Doctors’ views about training and future careers expressed one year after graduation by UK-trained doctors: questionnaire surveys undertaken in 2009 and 2010. BMC Med Educ 2014 Dec;14:270.
- 15. Kassim SS, McGowan Y, McGee H, Whitford DL. Prepared to practice? Perception of career preparation and guidance of recent medical graduates at two campuses of a transnational medical school: a cross-sectional study. BMC Med Educ 2016 Feb;16(1):56.
- 16. Alshishtawy M. Medical specialties in Oman: Scaling up through national action. Oman Med J 2009 Oct;24(4):279-287.
- 17. Al-Lamki N, Al-Lamki L. International accreditation of postgraduate medical education: Whither its role in Oman? Oman Med J 2016 Jan;31(1):1-4.
- 18. Sultan Qaboos University Student handbook [cited 2016 Dec 1]. Available from: https://www.squ.edu.om/Portals/6/TabModuleImages/COMHS%20Self-Study%20Book_%2031_3_2013.pdf .
- 19. FMHS undergraduate prospectus ebook [cited 2016 Dec 1]. Available from: http://ebooks.fmhs.auckland.ac.nz/mhsug-2017prospectus.
- 20. Oman Medical College Student handbook 2015-2016 [cited 2016 Dec 1]. Available from: http://www.omc.edu.om/Sohar/Medicine_Program.html#.
- 21. Hill J, Rolfe IE, Pearson SA, Heathcote A. Do junior doctors feel they are prepared for hospital practice? A study of graduates from traditional and non-traditional medical schools. Med Educ 1998 Jan;32(1):19-24.
- 22. Blitz J, Kok N, van Heerden B, van Schalkwyk S. PIQUE-ing an interest in curriculum renewal. Afr J Health Prof Educ 2014 May;6(1):23-27.
- 23. Chen CA, Kotliar D, Drolet BC. Medical education in the United States: do residents feel prepared? Perspect Med Educ 2015 Aug;4(4):181-185.
- 24. Dean SJ, Barratt AL, Hendry GD, Lyon PM. Preparedness for hospital practice among graduates of a problem-based, graduate-entry medical program. Med J Aust 2003 Feb;178(4):163-166.
- 25. Scicluna HA, Grimm MC, Jones PD, Pilotto LS, McNeil HP. Improving the transition from medical school to internship - evaluation of a preparation for internship course. BMC Med Educ 2014 Feb;14(1):23.
- 26. Illing J, Peile E, Morrison J, Morrow G, Davies C, Donaldson M, et al. How prepared are medical graduates to begin practice? A comparison of three diverse UK medical schools. Final Report for the GMC Education Committee. London: GMC; 2008.
- 27. Muthaura PN, Khamis T, Ahmed M, Hussain SR. Perceptions of the preparedness of medical graduates for internship responsibilities in district hospitals in Kenya: a qualitative study. BMC Med Educ 2015 Oct;15(1):178.
- 28. Gome JJ, Paltridge D, Inder WJ. Review of intern preparedness and education experiences in General Medicine. Intern Med J 2008 Apr;38(4):249-253.
- 29. Martin AA, Laurence CO, Black LE, Mugford BV. General practice placements for pre-registration junior doctors: adding value to intern education and training. Med J Aust 2007 Apr;186(7):346-349.
- 30. Dugan JP, Komives SR. Influences on college students’ capacities for socially responsible leadership. J Coll Student Dev 2010 Sep/Oct;51(5):525-549.