Puerperal hematomas can be seen in the vulva, vagina, or retroperitoneal regions, and incidence were reported as 1 in 300−1 000 deliveries.1 Episiotomy, instrumental delivery, vaginal lacerations, nulliparity, prolongation of second phase of labor, vulvar and vaginal varicose veins, and coagulopathies are the main risk factors in the etiology of puerperal hematoma.2 Clinical symptoms of the patients were perineal pain, swelling, or even hemorrhagic shock.3 The anatomic localization of bleeding is one of the main parameter for choosing the type of treatment.1,4
Case Report
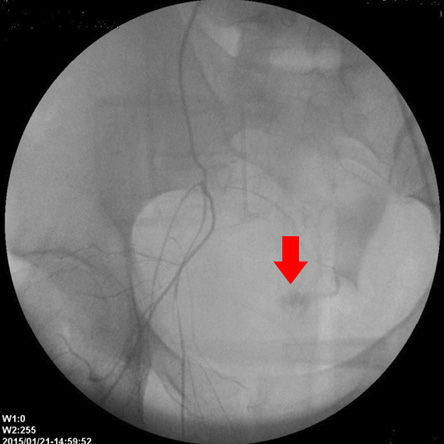
Figure 1: Angiography showed contrast extravasation at the right pudendal artery
(red arrow).
A 20-year-old primigravida patient was admitted to Istanbul Education and Research Hospital in the active phase of labor. She was in her 39th gestational week. Her history revealed no coagulopathy or previous surgical intervention. Her vital signs were blood pressure (BP) 120/60 mmHg, pulse rate 76 bpm (regular), and temperature 36 °C. External genitalia examination did not show any abnormality. Obstetric ultrasound (US) confirmed live single vertex presentation fetus. The estimated weight of the fetus was calculated as 3 010 g and the amniotic fluid volume was normal. Cardiotocography revealed reactive fetal heart beats, regular uterine contractions in sufficient severity, and spontaneous vaginal delivery was planned. Laboratory values revealed hemoglobin (Hb) value of 12 g/dL, hematocrit 37.3%, and platelet count 26 7000/mm3. After 14 hours of labor, right mediolateral episiotomy was performed and a baby girl with a weight of 3 100 g and a length of 51 cm was delivered. Placenta and attached membranes were fully delivered. No other laceration except episiotomy was detected on perineal examination. Episiotomy was primary sutured with continuous technique and no active bleeding was observed after the procedure. The patient had normal vital signs and she was closely followed for bleeding. After 20 minutes of delivery, the patient suffered pelvic pain radiating to the anus and felt vaginal pressure. The examination of external genitalia was normal, however, a painful mass approximately 7 × 8 cm extending from the right lateral fornix through the episiotomy line was palpated. The mass was diagnosed as a hematoma and no active bleeding was detected from the cervix. BP was 110/60 mmHg and heart rate was 76 bpm. Uterus was contracted on palpation and US examination revealed no free fluid. Complete blood count was performed and blood transfusion arrangement was done. The patient was prepared for surgery with intravenous crystalloid infusion. Episiotomy sutures were opened and nearly 500 cc hemorrhagic fluid was drained from hematoma which originated from right ischiorectal fossa. After Jackson-Pratt drain was inserted, the episiotomy incision was re-sutured. Foley catheter was placed in bladder and a firm gauze tampon was applied through to the vagina.
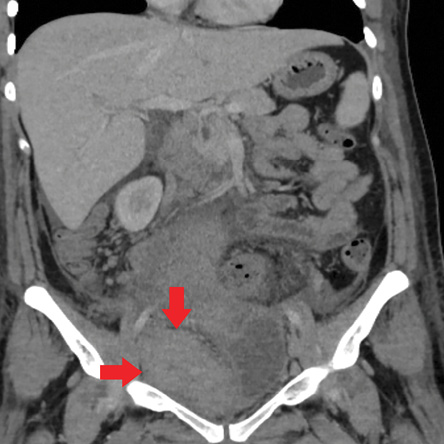
Figure 2: Computed tomography image after embolization hematoma in the right iliac fossa
(red arrows).
During post-operative care, hemorrhagic
500 cc fluid was collected from draining for two hours. The BP decreased to 80/50 mmHg and pulse rate increased to 112 bpm. The Hb level decreased to 7.1 g/dL and hematocrit was 22%. Serial transabdominal US demonstrated a hypoechoic lesion adjacent to the right wall of the vagina, which progressed to 10 × 11 cm diameter. Two units of erythrocyte suspensions, two units of fresh frozen plasma, and 500 mg tranexamic acid was infused. Then, emergent laparotomy was performed after that. Uterus, bilateral fallopian tubes, and ovaries were normal in the exploration.
There was hematoma in retroperitoneal region originating from subhepatic area, reaching to right iliac fossa and Douglas pouch. There was no bleeding from the bilateral uterine arteries and veins. Although bilateral hypogastric artery ligation was planned, it could not be performed because of active bleeding. We performed angiographic arteriography and embolization due to the bleeding. The surgical incision was closed anatomically. A 4F cobra catheter glide wire was inserted to the right internal iliac artery from the right femoral artery. During the procedure, extravasation from the right pudendal artery was observed [Figure 1]. No extravasation was seen from the left internal iliac artery and its branches. Bilateral iliac arteries were embolized by an injection of 15 cc gelfoam. The procedure was completed in 45 minutes without any complications.
The patient was admitted to the intensive care unit with stable hemodynamic parameters. Metronidazole and ceftriaxone empirical treatment was initiated. Two days after the operation, no drainage was observed in the pouch of Douglas and vaginal drainage tubes, hence they were removed. US and pelvic computed tomography (CT) examinations were performed during postoperative follow-up, which revealed a 7 × 10 cm sized hematoma extending from the right iliac fossa to the back of the uterus [Figure 2]. On the third day, the patient’s body temperature was measured at 39 °C and C-reactive protein (CRP) level was elevated to 13 mg/dL. It was thought that the fever was associated with hematoma. Blood, urine, and vaginal cultures did not demonstrate any microbial growth. On the sixth and tenth day, the US examinations revealed the regression of the hematoma. US guided percutaneous hematoma drainage was performed under local anesthesia. After this procedure, clinical and laboratory findings improved. The patient was discharged after 15 days. After four weeks, follow-up revealed no extraordinary pelvic US and laboratory findings.
Discussion
According to the localization of puerperal hematoma, it can be classified as vulvar, vulvo-vaginal, and retroperitoneal hematomas.1 Vulvar hematomas mostly occur as a result of injury to the branches of pudendal artery. Vaginal hematomas are usually caused by trauma to the descending branches of uterine artery.2,5
Retroperitoneal hematomas after delivery generally develops secondary to enlarged vaginal hematoma or uterine artery injury and uterine rupture.4,6 Also, vulvar hematoma secondary to spontaneous iliac artery rupture have been reported in the literature.7 According to our case, the hematoma was initially located at the vagina, subsequently extended to retroperitoneal area.
Symptoms mainly depends on the localization of hematoma and the amount of bleeding. Clinical presentations can vary from asymptomatic cases to hypovolemic shock and even death.1,2 In our patient, the pelvic pain spread to the anus.
Pelvic examination provides valuable important diagnostic information with US, CT, and magnetic resonance image (MRI).2,7 US can be effectively used in the diagnosis and follow-up of the patients, CT can be chosen in the diagnosis of arteriovenous malformations. MRI can be used especially in the evaluation of the extent of retroperitoneal hematomas and their relationship with other
pelvic organs.2,7,8
Puerperal hematomas may be treated conservatively, surgically, or angiographic arterial embolization. Unsuccessful bleeding control, progressive growth of hematoma, and failure to provide hemodynamic stability may require laparotomy and ligation of bleeding vessel or ligation of the internal iliac artery.9 In our case, emergent laparotomy was performed due to hemodynamic instability. Because of failure to explore the internal iliac artery, we moved on to the pelvic
angiographic embolization.
Pelvic angiographic embolization is an alternative treatment modality in the treatment of many obstetric and gynecologic hemorrhages. Use of arteriography in massive pelvic bleedings enables vascular mapping and selective artery embolization.10,11 In our case, we successfully applied selective artery embolization and had good response.
US guided aspiration of collections is a widely used technique. This method has many advantages like low risk adjacent organ injury, low cost and application with local anesthesia, and no need for radioactive agent.12,13 In the prevention of puerperal hematoma, it is important to begin the repair from the apex of perineal laceration or episiotomy suture leaving no dead tissue beneath and closely follow postpartum vital signs.14
Conclusion
Pelvic arterial angiography and embolization is a safe, tolerable, and minimally invasive treatment modality in the diagnosis and treatment of pelvic hemorrhage. It can be chosen as a first line treatment method in these cases rather than open surgery.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Chen TH, Chen CH, Hong YC, Chen M. Puerperal pelvic hematoma successfully treated by primary transcatheter arterial embolization. Taiwan J Obstet Gynecol 2009 Jun;48(2):200-202.
- 2. Guerriero S, Ajossa S, Bargellini R, Amucano G, Marongiu D, Melis GB. Puerperal vulvovaginal hematoma: sonographic findings with MRI correlation. J Clin Ultrasound 2004 Oct;32(8):415-418.
- 3. Scudamore JH. Vulval and vagınal haematomata. Br Med J 1964 May;1(5394):1357-1358.
- 4. Villella J, Garry D, Levine G, Glanz S, Figueroa R, Maulik D. Postpartum angiographic embolization for vulvovaginal hematoma. A report of two cases. J Reprod Med 2001 Jan;46(1):65-67.
- 5. Ridgway LE. Puerperal emergency. Vaginal and vulvar hematomas. Obstet Gynecol Clin North Am 1995 Jun;22(2):275-282.
- 6. Zahn CM, Yeomans ER. Postpartum hemorrhage: placenta accreta, uterine inversion, and puerperal hematomas. Clin Obstet Gynecol 1990 Sep;33(3):422-431.
- 7. Egan E, Dundee P, Lawrentschuk N. Vulvar hematoma secondary to spontaneous rupture of the internal iliac artery: clinical review. Am J Obstet Gynecol 2009 Jan;200(1):e17-e18.
- 8. Gondo S, Urushiyama D, Yoshizato T, Kora S, Maehara M, Kondo H, et al. The successful detection of postpartum unruptured vaginal pseudoaneurysm using ultrasonography: a case report. Springerplus 2014 Aug;3:482.
- 9. Lim PS, Nirmala CK, Shafiee MN, Lim YH, Rozman Z, Mohd HO,et al. Case Review: Postpartum vulvo-vaginal haematomas and options of management. Journal of Surgical Academia 2011;1(1):58-61.
- 10. Katz MD, Sugay SB, Walker DK, Palmer SL, Marx MV. Beyond hemostasis: spectrum of gynecologic and obstetric indications for transcatheter embolization. Radiographics 2012 Oct;32(6):1713-1731.
- 11. Singhal S, Singh A, Raghunandan C, Gupta U, Dutt S. Uterine artery embolization: exploring new dimensions in obstetric emergencies. Oman Med J 2014 May;29(3):217-219.
- 12. Del Cura JL, Zabala R, Corta I. [US-guided interventional procedures: what a radiologist needs to know]. Radiologia 2010 May-Jun;52(3):198-207.
- 13. Cohen M, Jacob D. [Ultrasound guided interventional radiology]. J Radiol 2007 Sep;88(9 Pt 2):1223-1229.
- 14. Dahdouh EM, Balayla J, Dubé J. Angiographic Embolization of a Postpartum Vulvovaginal Hematoma in a Patient with Situs Inversus Totalis: An Effective Second-Line Treatment. Case Rep Obstet Gynecol. 2013; 2013: 323781.