Nodular fasciitis (NF) is described as a benign, reactive, tumor-like lesion composed of fibroblasts and myofibroblasts.1,2 It typically occurs in the extremities and the trunk.2 The incidence of NF in the head and neck region is 13−20%.2−4 The exact etiology of the lesion is still unknown.However, preceding trauma is accepted as an important etiologic factor, but it is not present in every case.5–7 It appears as a firm, solitary nodule with an average diameter of 1−5 cm. It may extend into the subcutaneous tissue and the muscles.8,9 Because of its rapid-growing nature, clinically it is frequently misdiagnosed as an aggressive or a malignant lesion.5 This makes it important to diagnose NF correctly.
Here we report a case of NF located in the neck mimicking an invasive mass of the thyroid gland.
Case Report
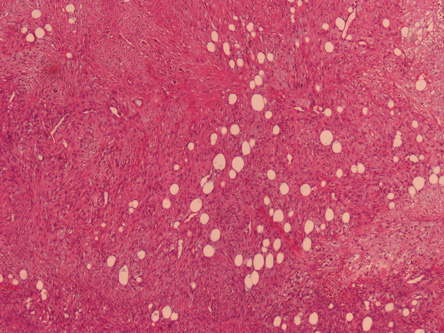
Figure 1:Hematoxylin and eosin staining showing plump, spindle-shaped cells arranged in short, irregular bundles and fascicles intermixed with adipose tissue in myxoid and some fibrous matrix in nodular fasciitis. Magnification = 40 ×.
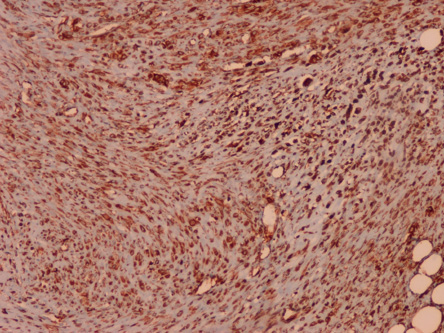
Figure 2: SMA positive immunostaining of cells of nodular fasciitis. Magnification = 40 ×.
An 82-year-old woman was admitted to the emergency department with a one-month history of progressive shortness of breath. In the emergency room, a tracheostomy was performed and an invasive mass to the trachea, thought to evolve from thyroid gland, was discovered.
The clinical findings prompted us to think about the following differential diagnoses: thyroid malignancies, soft tissue malignancies, and malignant trachea tumors. An incisional biopsy was done. Two biopsies with diameters of 1 cm and 5 cm were taken. They were solid, firm, and grey-white in color.
Hematoxylin and eosin (H&E) stained slides were prepared and immunohistochemical (IHC) panel for vimentin (VIM), smooth muscle actin (SMA), desmin, CD10, CD34, CD68, leukocyte common antigen (LCA), chromogranin, S-100, cytokeratin (CK), B-cell lymphoma 2 (Bcl-2), thyroid transcription factor-1 (TTF-1), epithelial membrane antigen (EMA), calretinin, and calponin were performed.
Microscopic examination of the H&E slides revealed plump, spindle-shaped cells with oval, pale-staining nuclei, and prominent nucleoli arranged in short, irregular bundles and fascicles intermixed with adipose tissue in myxoid and some fibrous matrix [Figure 1]. Some nuclei showed hyperchromasia, pleomorphism, and mitosis. Extravasated erythrocytes, well-formed capillaries, and multinucleated giant cells were also present. VIM, SMA [Figure 2], calponin [Figure 3], and CD10 [Figure 4] were positive confirming NF. CD34 IHC showed many capillaries through the lesion.
As the lesion was invasive to the trachea, it was not possible to excise only the mass, and a total laryngectomy had to be performed, but the age and general status of the patient was not suitable for a major operation. An intralesional corticosteroid injection was administered; however, no response was obtained.
To prevent progressive shortness of breath, (17 dose) radiotherapy was given to the patient as a last resort treatment, but a major response was not seen in the mass. The therapy was terminated as the general status of the patient worsened. She is now followed-up without any therapy.
Discussion
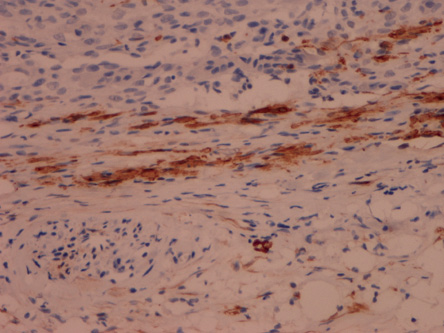
Figure 3: Calponin positive immunostaining of cells of nodular fasciitis. Magnification = 100 ×.
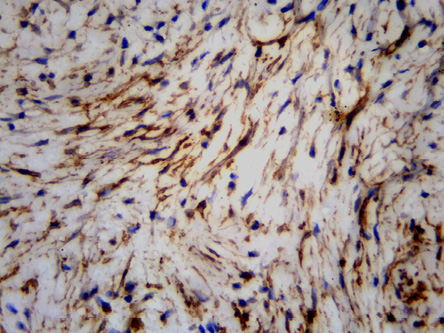
Figure 4: CD10 positive immunostaining of cells of nodular fasciitis. Magnification = 100 ×.
NF is a benign soft tissue lesion composed of tumor-like fibroblastic and myofibroblastic proliferation. It is also known as subcutaneous pseudosarcomatous fibromatosis, infiltrative fasciitis, or proliferative fasciitis.10,11 The etiology is still unknown, but it is thought to occur due to the unusual proliferation of myofibroblasts triggered by local injury or inflammatory process.8,11 Although NF may occur in patients of any age, it is most common in adults 20 to 40 years old. Only 14% of the patients are < 10 or > 60 years old. The sex distribution is equal.4 Although it may occur virtually anywhere on the body, the majority of the cases present as superficial soft tissue masses in the extremities or trunk. Only 13−20% of cases occur in the head and the neck region.2–4 NF has also been reported in a variety of unusual locations, including the parotid gland, external ear, oral cavity, breast, and lymph node capsule.4 It is one of the most difficult lesions to diagnose because it can be confused with spindle cell sarcoma, fibromatosis, fibrous histiocytoma, nerve sheath tumors, and pleomorphic adenomas. It has a short history, rapid growth, marked infiltrative margins, and similar histopathological appearance.2,11 It usually presents as a solitary, painless, and rapidly growing nodule of less than three months duration with a diameter of 1−5 cm.8,11 The macroscopy of NF is dependent on the relative amounts of myxoid, fibrous stroma, and the cellularity of the lesion. It is nonencapsulated; however, most are well circumscribed, particularly those located near the deep fascia, which infiltrate the surrounding soft tissues.
NF has three subtypes according to its relation to the fascia: subcutaneous, intramuscular, and fascial. The most common form is the subcutaneous type, which is a well-circumscribed spherical nodule attached to the fascia, growing upward into the subcutis. The intramuscular type locates in the muscles as an ovoid, larger mass, and attaches to the fascia. The fascial type locates along the fascia and it is the least well-circumscribed as it grows along the interlobular septa of the subcutaneous fat.4
All NF types are composed of plump, immature-appearing fibroblasts and myofibroblasts arranged in short, irregular bundles and fascicles in a fibrous and/or myxoid stroma. The cells have oval, pale nuclei with prominent nucleoli. Typical mitosis are common. Some lymphoid cells, erythrocytes, well-formed capillaries, a small number of lipid macrophages, and multinucleated giant cells can be seen through the lesion.4,8,11 Sometimes a few histologic variations can be seen in the subtypes. The intramuscular type may contain residual atrophic muscle fibers and muscle giant cells. In the fascial type, cells may arrange in a radial fashion around a central, poorly cellular, edematous area containing mucoid material and fibrin. The microscopic appearance changes according to the preoperative duration of the lesion. Younger lesions tend to have predominantly myxoid stroma, whereas old lesions have hyaline fibrosis, tissue shrinkage, and minute fluid-filled microcysts. In cases of long duration, when the microcysts fuse and form a large centrally located cyst, the lesion can be named cystic NF.4
In the immune profile of NF, myofibroblasts stain for SMA, muscle-specific actin (MSA), and VIM. Desmin is rarely expressed, and S-100 and CK are negative, different from neural and epithelial lesions.4 Morgen et al12 stated that calponin, CD10, and protein gene product 9.5 (PGP9.5) were positive in their cases of head and neck NF in addition to SMA. We also found that calponin and CD10
were positive in our case staining fibroblastic or myofibroblastic cells. h-Caldesmon expression can be used to distinguish smooth muscle from myofibroblastic proliferation, and β-catenin may be useful as it is expressed in fibromatoses different from NF. CD56 can help to rule out neural tumors, leiomyoma, leiomyosarcoma, and low-grade myofibroblastic sarcoma in which the marker is
often positive.12
As in our case, NF can cause emergencies depending on the localization of the lesion. For instance, rapidly growing NF originating from the external auditory canal may cause obstruction, pain, and drainage,13 and NF localized in pelvis, retropubic space may cause cystitis-like symptoms and macroscopic hematuria.14
The preferred treatment for NF is local excision. Recurrence is rare as it has a good prognosis and metastases do not occur. Rare spontaneous regression and rapid resolution with intralesional corticosteroid injection in lesions that cannot be excised completely have been reported.8,9,15 In addition, radiotherapy has been reported to be the last therapy option for this disease in other vital organs such as the eyes. 16,17
In our case, the lesion was attached to the thyroid gland and caused depression of the trachea resulting in progressive shortness of breath. The clinicians believed the lesion was an aggressive tumor originating from the thyroid gland, the trachea, or soft tissues.
Conclusıon
NF is a histologically and clinically diverse lesion that creates diagnostic confusion as it can behave like an aggressive malignancy. Histology-based differential diagnoses includes a large number of lesions and tumors especially when the lesion contains more mitoses, giant cells, mild nuclear atypia, and hypercellularity. Clinicians should remember that NF may cause airway obstruction in a similar way to an aggressive malignant tumor. Thus, it is important to diagnose NF correctly to avoid unnecessary additional surgery and treatment.
Disclosure
The authors declared no conflicts of interest.
Acknowledgements
The authors wish to thank Associate Professor. Mine Tunakan Öztop for her diagnostic support.
references
- 1. Thompson LD, Fanburg-Smith JC, Wenig BM. Nodular fasciitis of the external ear region: a clinicopathologic study of 50 cases. Ann Diagn Pathol 2001 Aug;5(4):191-198.
- 2. Al Rahbi M, Al-Kindi H, Al-Sheibani S. Post-aural Nodular Fasciitis. Oman Med J 2015 Jan;30(1):63-65.
- 3. Montgomery EA, Meis JM. Nodular fasciitis. Its morphologic spectrum and immunohistochemical profile. Am J Surg Pathol 1991 Oct;15(10):942-948.
- 4. Goldblum JR, Folpe AL, Weiss SW. Enzinger and Weiss Soft tissue tumors, 6th ed. Elsevier, Saunders, 2014.
- 5. Majidi MR, Jafarian AH, Irani S. Nodular fasciitis of the auricle: a case report. Iran J Otorhinolaryngol 2013;25(71):115-118.
- 6. Nishi SP, Brey NV, Sanchez RL. Dermal nodular fasciitis: three case reports of the head and neck and literature review. J Cutan Pathol 2006 May;33(5):378-382.
- 7. Konwaller BE, Keasbey L, Kaplan L. Subcutanous Pseudosarcomatous Fibromatosis (fasciitis). Report of 8 cases. Am J Clin Pathol 1995;25:241-252.
- 8. Cyriac MJ, Celine MI, Kurien G, Puthiode U. Nodular fasciitis. Indian J Dermatol Venereol Leprol 2004 Jul-Aug;70(4):239-241.
- 9. Graham BS, Barrett TL, Goltz RW. Nodular fasciitis: response to intralesional corticosteroids. J Am Acad Dermatol 1999 Mar;40(3):490-492.
- 10. Koenigsberg RA, Faro S, Chen X, Marlowe F. Nodular Fasciitis as a Vascular Neck Mass. AJNR 1996;17:567-569.
- 11. Singh S, Paul S, Dhall K, Khichy S. Nodular fasciitis: a diagnostic challenge. Indian J Pathol Microbiol 2013 Jul-Sep;56(3):288-290.
- 12. Morgen EK, Carter P, Weinreb I, Al-Habeeb A, Ghazarian DM. Immunohistochemistry in nodular fasciitis of the head and neck. Pathology 2013 Jun;45(4):432-433.
- 13. Milo AG, Vito KJ, Kinney SE, Bauer TW. Nodular fasciitis arising in the external auditory canal. Otolaryngol Head Neck Surg 1999 Apr;120(4):591-592.
- 14. Matsuta Y, Moriyama N, Oyama N, Miwa Y, Akino H, Yokoyama O, et al. [Nodular fasciitis arose in the pelvis : a case report]. Hinyokika Kiyo 2010 Jan;56(1):35-39.
- 15. Odom RB, James WD, Berger TG. Andrew’s Diseases of the Skin: Clinical Dermatology. 9th ed. Philadelphia: WB Saunders 2000.
- 16. Shields JA, Shields CL. Tumors of the conjunctiva. In: Eyelid, conjunctival, and Orbital Tumors: An atlas and textbook. 2nd ed. Wolters Kluver- Lippincott Williams and Wilkins; 2008. p. 374.
- 17. Lommatzsch PK, Werschnik C. Conjunctival tumors and their treatment by radiotherapy. In: Sagerman RH, Alberti WE, editors. Radiotherapy of intraocular and orbital tumors. 2nd ed. Springer, 2003. p. 182.