Platelet count estimation is an important element of the diagnostic and treatment process in many disorders. In patients with thrombocytopenia, especially when platelet transfusion is considered, the reliability of platelet estimation is essential to make clinical decisions.1 Although hematology analyzers provide reliable full blood counts based on their linearity limits, they are known to be inaccurate and poorly reproducible at enumerating platelets in severe thrombocytopenia.2 The inaccuracies can be secondary to interference from cells or materials of a similar size to platelets, which may influence the automated measurement using hematology analyzers.3 Therefore blood films have been commonly used for platelet estimation in settings of low platelet count. Beside manual estimation of platelet count, blood film evaluation provides additional assessment of platelet size, shape, granulation, and analysis of phenomena such as aggregation or platelet satellitism.
Manual platelet estimation using various methods in severe thrombocytopenia cases is more accurate compared to automated methods.2,4 However, the reproducibility of manual platelet counting has not been adequately studied.
The objective of this study was to assess the reproducibility of manual platelet estimation when the platelet count was below 100 × 109/L, and to evaluate the impact of the level of experience of the individual counting on the reproducibility of manual platelet estimate.
Methods
This cross-sectional study was conducted over a period of four months (July to November 2014) at Sultan Qaboos University Hospital. We enrolled 136 consecutive patients and had total data for 101 patients. Patients with a platelet count less than 100 × 109/L, which was determined using the automated optical hematology analyzers CELL DYN Sapphire™ (Abbott Diagnostics, USA) during complete blood count, were included in the study. Peripheral blood films were obtained and stained with Wright-Giemsa stain. Cases with pseudothrombocytopenia due to platelet aggregation or platelet satellitism were excluded. There were no specific diseases or conditions considered for exclusion in the study.
Sample collection and processing was uniform in the study. The blood films were given to four laboratory scientists with different levels of experience: a junior scientist (R1), a hematology resident (R2), and two senior scientists (R3, R4). Each rater performed an independent manual platelet estimate for each blood film. All raters were blinded to the automated platelet count and other raters estimates. All raters used a standardized protocol to determine platelet count. This involved determining an average platelet count in 10 high power fields using 100× objective and multiplying the average by 20.5
Continuous variables are presented as mean with standard deviation (SD) or as median with interquartile range (IQR). For the purpose of analyzing the impact of the level of experience, raters were ordered according to the level of experience with R1 being the least experienced and R4 being the most experienced. The agreement in the manual platelet count estimate among the raters was assessed using two methods: the intraclass correlation coefficient (ICC) and modified Bland-Altman plots.6 The correlations between the raters were assessed using Spearman’s correlation coefficient. We used linear regression to assess the impact of the baseline characteristics (platelet count estimate, hemoglobin level (Hb), and mean corpuscular volume (MCV)) on the disagreement in the platelet count estimate. Kruskal-Wallis equality-of-populations rank test with alpha threshold of 0.050 was used for ICC comparison of the different rater pairs. To detect a minimum correlation of 0.30 with a power of 90% and one-sided alpha of 0.05, 93 samples were required.7,8 To compensate for any missing data, we included 100 samples. Data were analyzed using STATA 13 software (StataCorp. 2013, Texas, US). The study was reviewed and approved by the Ethics Committee of the College of Medicine and Health Sciences (MREC#787).
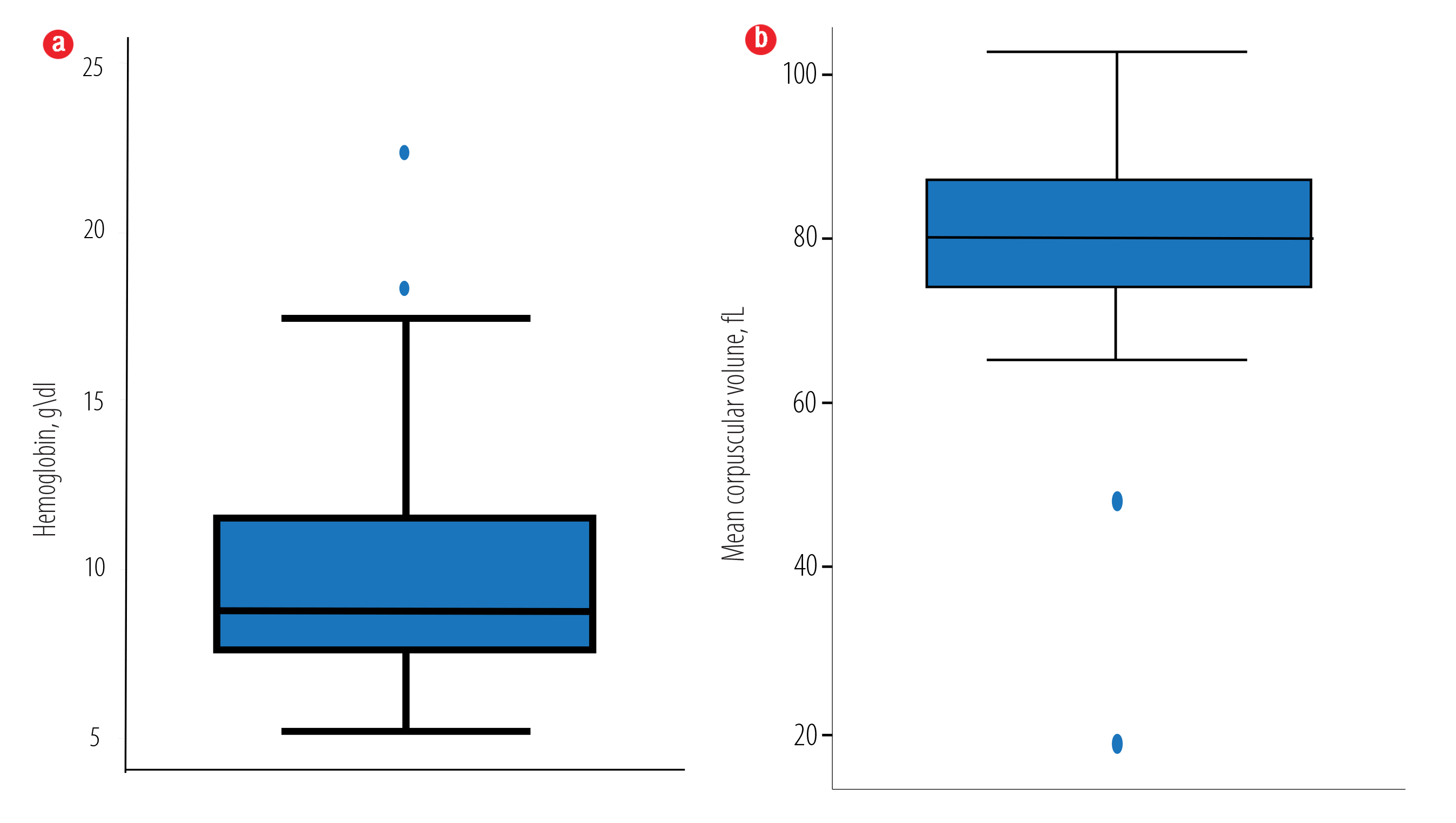
Figure 1: Baseline (a) hemoglobin (Hb) and (b) mean corpuscular volume (MCV) characteristics for the 100 complete blood counts. The mean Hb and mean MCV of the included samples (n = 100) were 9.8 ± 3.3 g/dL and 80.5 ± 11.2 fL, respectively.
Table 1: Pair rater manual platelet counts correlation between the different raters (R) in the study.
|
R1 |
1.000 |
|
|
|
|
R2 |
0.984 |
1.000 |
|
|
|
R3 |
0.845 |
0.862 |
1.000 |
|
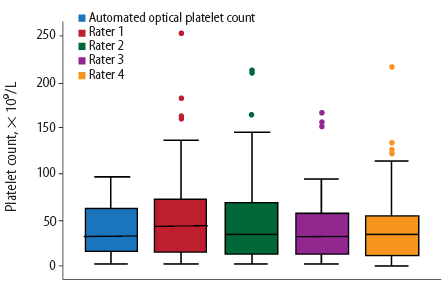
Figure 2: Box plot distribution of the estimated platelet count using the automated optical method and manual platelet estimates by raters 1 to 4.
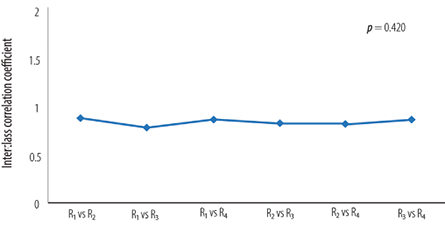
Figure 3: Comparison of intraclass correlation coefficient (ICC) among different paired raters. Raters were ordered in increasing level of experience: a junior scientist (R1), a hematology resident (R2), and two senior scientists (R3, R4)
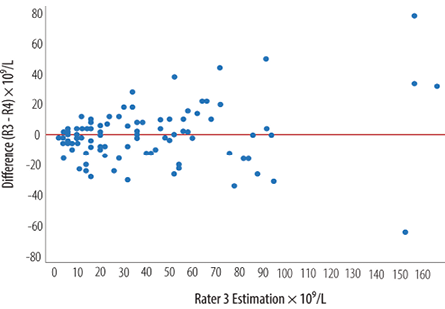
Figure 4: Modified Bland-Altman Plot comparing the two most experienced raters (R3 vs. R4). Differences in platelet estimation, as indicated by the distance between the dots, were small with lower platelet estimate but increased with increasing platelet estimate.
Results
The mean Hb and mean MCV of the included samples were 9.8±3.3 g/dL and 80.5±11.2 fL, respectively. The mean automated optical platelet count estimate was 40±30 × 109/L [Figure 1]. The mean manual platelet count estimates by the four raters were 51±44 × 109/L, 48±45 × 109/L, 40±35 × 109/L, and 40±36 × 109/L, respectively [Figure 2]. Spearman’s correlation among different rater pairs ranged from 0.84 to 0.89, indicating a strong correlation [Table 1]. The overall ICC was 0.84 indicating excellent agreement. The pair-wise comparison of the ICCs of the raters (when the pairs were ordered in increasing level of experience) showed no statistically significant difference between the different ICCs (p = 0.420) [Figure 3]. Comparing the two most experienced raters (R3 and R4), the differences in the manual platelet count estimate was small when the count was low but increased with higher platelet count [Figure 4]. The differences ranged from -64 to 78 × 109/L with a median of zero (IQR -10, 8). The platelet estimate by the lesser-experienced rater was the only baseline predictor of disagreement (p = 0.037).
Discussion
To the best of our knowledge, this is the first study to assess the reproducibility of manual platelet counts in patients with platelet counts less than 100 × 109/L. We have demonstrated that manual platelet count estimate is reproducible in trained competent hands when using a standardized methodology. We have also shown that the difference in manual platelet count increases with increased platelet count and the level estimated by a less experienced rater predicts this difference. The correlation among different pairs of raters is strong.
The use of a standardized manual platelet count has likely led to the high reproducibility of the estimate in our study. When reproducibility of automated manual platelet count was evaluated using a standard method, it was much lower.9,10 The UK National External Quality Assessment Service. (UK NEQAS) distributed 29 external quality specimens with platelet counts less than 64 × 109/L to more than 1100 users of 23 different hematology analyzers. The majority of the automated analyzer results overestimated the platelet count with significant differences in 16.5% of cases.9 Another study evaluated 403 samples with platelet counts less than 50 × 109/L with various hematology analyzers using optical and impedance methods. All methods showed a positive bias, especially at levels less than 20 × 109/L, resulting in an undertransfusion risk of 9.1%.10 Unfortunately, we did not find studies addressing our question to compare to our results to.
The strong correlation between different pairs of raters with different levels of experience was expected when using a standardized methodology for estimation. However, this does not equal good reproducibility as it simply means that the estimate had a similar increase by one rater when the estimate of the other increased. We have included it in our study, in addition to the ICC, because it gave another quality characteristic of the manual platelet count and corroborated with the findings from the ICC analysis.
When comparing the different pairs, the ICC does not change with varying levels of experience. This is a reassuring finding and gives an indication that junior laboratory scientists can perform manual platelet counts provided they have been trained and deemed competent to perform the standardized methodology used in our study. This conclusion may not be true for other methodologies (e.g., using a smaller number of fields) unless it is studied specifically. The modified Bland-Altman plot shows that the differences are small with a median that is close to zero and a narrow IQR. However, the differences increase with increasing platelet estimates between the two most experienced raters. This is also shown when using regression methods to predict the differences. In the multivariable linear regression model, the only significant predictor is the platelet count (estimated by the lesser experienced rater). It is unlikely that the level of experience plays an important role here given the lack of the difference in ICC among different raters. Although, the MCV may be important in predicting the differences when using automated platelet count,1,11 this is not true with manual platelet count estimation.
One study limitation is the lack of a gold standard (like CD61 based platelet estimate) to assess the accuracy of the obtained results. That said, the objective of this study was to assess the reproducibility and not the accuracy. Moreover, we chose a cut-off level of 100 × 109/L for inclusion into the study, which may not have been appropriate. To determine if the reproducibility was less with a lower platelet count, we would need to have a larger sample size to be able to stratify according to different levels of platelet count and assess the reproducibility at each level. Other factors that could potentially impact reproducibility, and were not included in our study, are the underlying primary disease, platelet volume, and method of blood film preparation. One strength of this study is its methodology in using a standardized protocol by different independent raters who are blinded to the automated platelet count and the estimate from the other raters.
Conclusion
It is crucial for any standard of care test to be reproducible. Manual platelet counting is a standard of care in cases of thrombocytopenia, and our study has demonstrated that manual platelet count estimation is reproducible. For future confirmation of these findings, we plan for a larger prospective study using CD61 as a gold standard method and investigation using a different number of high power fields and cut-off values.
Disclosure
The authors declared no conflicts of interest. The project was supported by a grant from the Graduate Research Support Program (GRSP), The Research Council (TRC).
Acknowledgements
We would like to thank our colleagues from the Hematology Department at the Sultan Qaboos University Hospital for their expertise, which greatly assisted this research.
references
- 1. Pinkowski R. Difference between impedance and optical platelet count methods in patients with microcytosis of red blood cells. Lab Hematol 1999;5:22-27.
- 2. Segal HC, Briggs C, Kunka S, Casbard A, Harrison P, Machin SJ, et al. Accuracy of platelet counting haematology analysers in severe thrombocytopenia and potential impact on platelet transfusion. Br J Haematol 2005 Feb;128(4):520-525.
- 3. Hong KH, Kim MJ, Lee KW, Park KU, Kim HS, Song J. Platelet count evaluation using three automated haematology analysers compared with the immunoplatelet reference method, and estimation of possible inadequate platelet transfusion. Int J Lab Hematol 2009 Jun;31(3):298-306.
- 4. Oliveira RA, Takadachi MM, Nonoyama K, Barretto OC. Is automated platelet counting still a problem in thrombocytopenic blood? Sao Paulo Med J 2003 Jan;121(1):19-23.
- 5. Rodak BF, Fritsma GA, Doig K. Hematology: Clinical principles and applications. 4th ed. Elsevier-Saunders; 2011. p. 202
- 6. Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess 1994;6(4):284-290.
- 7. Dancey CP, Reidy J. Statistics Without Maths for Psychology: Using SPSS for Windows. Pearson Education. New York: Prentice Hall; 2004.
- 8. Portney LG, Watkins MP. Foundations of clinical research: applications to practice (Vol. 2). Upper Saddle River, NJ: Prentice Hall; 2000. p. 560-567.
- 9. De la Salle BJ, McTaggart PN, Briggs C, Harrison P, Doré CJ, Longair I, et al. The accuracy of platelet counting in thrombocytopenic blood samples distributed by the UK National External Quality Assessment Scheme for General Haematology. Am J Clin Pathol 2012 Jan;137(1):65-74.
- 10. Marionneaux S, Francisco N, Chan V, Hanenberg J, Rafael J, Chua C, et al. Comparison of automated platelet counts and potential effect on transfusion decisions in cancer patients. Am J Clin Pathol 2013 Nov;140(5):747-754.
- 11. Briggs C, Kunka S, Machin SJ. The most accurate platelet count on the Sysmex XE-2100. Optical or impedance? Clin Lab Haematol 2004 Apr;26(2):157-158.