|
Introduction
A 38-year-old female presented with a longstanding painless swelling overlying the scapula on the right side and has been gradually increasing in size with occasional episodes of pain radiating to the right arm. The clinical diagnosis was a soft tissue tumor. MRI was reported as suggestive of irregular fibro-fatty tissue with muscular infiltration and inflammation. Fine needle aspiration (FNA) retrieved a paucicellular aspirate with a few clusters of adipocytes. The diagnosis was a lipomatous lesion and excision was advised for histopathological examination. The intraoperative findings showed the tumor located deep into the rhomboids and latissimus dorsi and extending deep into the right scapula. The excised specimen was sent for histopathological examination.
Macroscopically, the specimen was an irregular, lobulated soft tissue mass weighing 209 grams and measuring 11×10×5.5 cm. Serial slicing of the specimen showed greyish white and fatty tissue admixed with hemorrhagic tissue. There was no evidence of necrosis, calcification or cystic change. The microscopic picture of the lesion is shown in Fig 1.
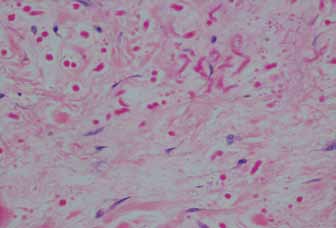
Figure 1: Hematoxylin and eosin (H&E) stain, deeply eosinophilic serrated or beaded bands and globoid structures seen in collagenous stroma (×20).
Questions
1. What is the diagnosis?
a) Fibromatoses
b) Nuchal fibroma
c) Elastofibroma
d) Fibrolipoma
2. Which special stain helps in the diagnosis?
a) Masson’s trichrome
b) Elastic-Van-Gieson
c) Periodic acid Schiff
d) Verhoff ’s
Answers
1. Elastofibroma
2. Elastic-Van-Gieson
Discussion
Jarvi and Saxon first described this rare entity in 1961.1 This is a slow growing benign soft tissue tumor with a marked predilection for women and seen in the elderly.1 But cases have been reported in the age group ranging from 35-94 years. In 99% of the cases, they are located in the inferior subscapular region.2 It is called elastofibroma dorsi when it occurs in the periscapular region. Other uncommon locations include the deltoid muscle, ischial tuberosity, greater trochanter, foot, olecranon process, thoracic wall, stomach, mediastinum, orbit, cornea and the oral mucosa.1
Elastofibroma is characterised by the accumulation of abnormal elastic fibres and hence it is generally regarded as a reactive process. It can be considered an unusual fibroblastic pseudotumor.1 The pathogenesis of the lesion remains unclear, but long standing repeated trauma to the tissues between the scapula and chest wall may cause the reactive hyperproliferation of fibroelastic tissue.2 An increased prevalence is seen in persons with a history of manual labor using the shoulder girdle, probably traumatic.3 Another theory is the non-traumatic origin where genetic factors are considered to be responsible. These cases have a positive family history.4 Affected patients may show elastofibroma-like changes at a visceral location suggesting genetic predisposition.5 The histogenesis of the elastic fibres is controversial. They result from elastotic degeneration of the collagen fibres or could be a product of abnormal elastogenesis or even a combination of both processes. There is much debate over whether they are truly elastic fibres. But there is evidence that it is truly elastin which is most likely derived from the periosteal cells.6
Elastofibromas generally present as painless swellings. A few cases are associated with pain or snapping of the scapula. In a few cases, they are found bilaterally.7 The differential diagnoses include nuchal fibroma, fibrolipoma, fibromatoses, sarcoma and subcutaneous metastasis. Ultrasonographically, the lesions show a lternating pattern of hyperechogenic and hypoechogenic lines.8 MRI is the investigation of choice, as they show an alternating pattern of fibrous and fatty tissue reflecting entrapped fat within a fibrous mass. CT is less sensitive for visualising the fatty tissue and appears as a homogenous mass with a density inferior to that of muscle.7 Preoperative procedures like fine needle aspiration are not successful as the lesions are hypocellular.1
Surgical treatment is reserved for symptomatic cases only.3 Histologically, they are dermal, unencapsulated, hypocellular masses composed of fibro collagenous strands mixed with fat. The collagenous areas showed plump/spindle-shaped nuclei with fine chromatin. Deeply eosinophilic serrated or beaded bands and globoid structures are seen scattered in the collagenous areas. These fibres are difficult to detect with haematoxylin and eosin staining especially during frozen sections. They stain positively with elasticstain (Elastica-van-Gieson [Fig. 2]). Immunohistochemically, elastofibromas stain positively for Vimentin but negatively for smooth muscle actin, S-100, desmin and p53. They are frequently positive for CD34 and lysozyme. On ultrastructural examination, the elastic fibres appear as granular or fibrillary aggregates of electron-dense material surrounded by an amorphous matrix with scattered microfibrils.6
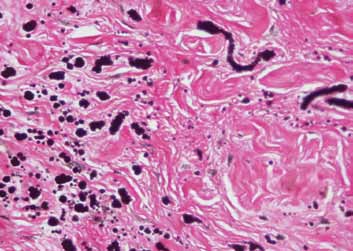
Figure 2: Elastica-Van-Gieson stain highlights the beaded and globular elastic fibres (× 20).
Elastofibroma can be differentiated from the above mentioned conditions by the absence of elastic fibres. Immunohistochemically, they show the following staining patterns. Nuchal fibroma is positive for Vimentin, CD34 and CD99. Fibrolipoma shows only CD34 staining; while, fibromatoses shows Vimentin positivity, but is negative for CD34. Sarcomas show a wide range of staining patterns. They show CD34, Vimentin, reticulin, p53 and high Ki67 positivity.
Elastofibroma is a rare soft tissue lesion. Located at this specific site, it should be considered as a likely diagnosis. Elastofibroma is included in the differential diagnoses of the chest wall tumors. Surgical resection is considered only in symptomatic patients. The MRI features of elastofibroma are different from those of most other soft tissue tumours, reflecting entrapped fat within a predominantly fibrous mass suggesting a presumptive diagnosis of elastofibroma. FNA and frozen section are not helpful.
Acknowledgements
The authors reported no conflict of interest and no funding wa sreceived for this work.
References
1. Robert A. Schwartz, Sonja Stander, Thomas Schwarz. Elastofibroma:Dermatology article 2011. Available at: http://emedicine.medscape.com/article105711
2. Daigeler A, Vogt PM, Busch K, Pennekamp W, Weyhe D, Lehnhardt M, etal. Elastofibroma dorsi–differential diagnosis in chest wall tumours. World JSurg Oncol 2007;5:15.
3. Fletcher.C D M. Soft tissue tumors. In: Diagnostic Histopathology ofTumours. 3rd ed. Churchill Livingstone: Elsevier,2007. 1542-43p
4. Vanni R. Soft tissue tumors: Elastofibroma. Atlas Genet Cytogenet OncolHaematol. November 2003.
5. Enjoji M, Sumiyoshi K, Sueyoshi K. Elastofibromatous lesion of the stomachin a patient with elastofibroma dorsi. Am J Surg Pathol 1985 Mar;9(3):233-237.
6. Kumaratilake JS, Krishnan R, Lomax-Smith J, Cleary EG. Elastofibroma:disturbed elastic fibrillogenesis by periosteal-derived cells? Animmunoelectron microscopic and in situ hybridization study. Hum Pathol1991 Oct;22(10):1017-1029.
7. Rosai & Ackermans. Soft tissues. In: Surgical Pathology. 9th ed. Mosby:Elsevier,2004. 2247-48p
8. Muratori F, Esposito M, Rosa F, Liuzza F, Magarelli N, Rossi B, et al.Elastofibroma dorsi: 8 case reports and a literature review. J OrthopTraumatol 2008 Mar;9(1):33-37.
|