Comparing Serum Follicle-Stimulating Hormone (FSH)
Level with Vaginal PH in Women with Menopausal
Symptoms
Fatemeh Vahidroodsari,1 Seddigheh Ayati,1 Zohreh Yousefi,1 Shohreh Saeed2
Vahidroodsari F, et al. OMJ. 25, 13-16 (2010); doi:10.5001/omj.2010.4
ABSTRACT
Objectives: Despite the important implication for women’s health and reproduction, very few studies have focused on vaginal PH for menopausal diagnosis. Recent studies have suggested vaginal PH as a simple, noninvasive and inexpensive method for this purpose. The aim of this study is to compare serum FSH level with vaginal PH in menopause.
Methods: This is a cross-sectional, descriptive study, conducted on 103 women (aged 31-95 yrs) with menopausal symptoms who were referred to the Menopausal Clinic at Ghaem Hospital during 2006. Vaginal pH was measured using pH meter strips and serum FSH levels were measured using immunoassay methods. The data was analyzed using SPSS software (version 11.5) and results were evaluated statistically by the Chi-square and Kappa tests. p≤0.05 was considered statistically significant.
Results: According to this study, in the absence of vaginal infection, the average vaginal pH in these 103 menopausal women was 5.33 ±0.53. If the menopausal hallmark was considered as vaginal pH>4.5, and serum FSH as ≥20 mIU/ml, then the sensitivity of vaginal pH for menopausal diagnosis was 97%. The mean of FSH levels in this population was 80.79 mIU/ml.
Conclusion: Vaginal pH is a simple, accurate, and cost effective tool that can be suggested as a suitable alternative to serum FSH measurement for the diagnosis of menopause.
From the 1Department of Obstetrics and Gynecology, Women’s Health Researches Center, Mashhad University of Medical Sciences, Iran, 2Department of Obstetrics and Gynecology, Birjand University of Medical Sciences, Iran.
Received: 09 Nov 2009
Accepted: 22 Dec 2009
Address correspondence and reprint requests to: Dr. Seddigheh Ayati, Department of Obstetrics and Gynecology, Ghaem Hospital, Women’s Health Research Center, Mashhad University of Medical Sciences, Iran. E-mail:ayatis@mums.ac.ir
INTRODUCTION
Menopause is the physiological cessation of menstruation which usually has a negative impact on the quality of life of most women.1 It begins twelve months after the last menstruation and it is demonstrated by elevated levels of follicle-stimulating hormone (FSH). The average age of menopause has not changed from 600 B.C, the mean age has been 51.4±3.8 yrs.2,3 In a study conducted by the "National Health Center ", it was reported that the average age of menopause among Iranian women was 49.6 yrs, while among U.S women the average age of menopause was 51±1 yrs.4 Increase in serum FSH, with or without a decrease of estradiol, has been observed in women over the age of 40 yrs who continue to cycle regularly.5 Moreover, abrupt fluctuation in serum FSH and estradiol may also be observed with postmenopausal levels returning to the normal reproductive range.6
Menopause is diagnosed by age, cessation of menstruation for more than one year and presence of symptoms. FSH can be used to confirm the diagnosis in the presence of the above and may not be necessary in most cases. Although recently, some studies have proposed vaginal pH as another method for this purpose.5 It has been known for decades that without vaginal infections, vaginal pH is ≤4.5 during the reproductive years and >4.5 before menarche and after menopause. Contamination with cervical mucus, blood or semen leads to incorrect vaginal pH interpretation.7
There is a relationship between sufficient vaginal estrogen and the vaginal micro-organism and their metabolic products.8,9 In response to estrogen, vaginal epithelial cells proliferate, their glycogen content is increased and subsequently, lactobacillus produces lactic acid from glycogen and causes an acidic pH which maintains vaginal health.10 In the presence of vaginitis, vaginal pH of >4.5 may indicate various infections such as bacterial vaginosis, trichomonas vaginalis, group B streptococcus or other pathogenic organisms.11 In the absence of vaginitis, an elevated vaginal pH may reflect low circulating estrogen levels (estradiol <40 pg/ml) or inadequate response of atrophic vaginal epithelium to estrogen therapy.12
However, like an elevated temperature at the time of ovulation, an elevated pH alone is only presumptive and not diagnostic. Menopause can be recognized by elevated serum FSH level, before the onset of symptoms. But this is an expensive test, and according to the patient's socioeconomic status, it is reasonable to choose a more cost effective, simple and noninvasive method.13 Some authors have suggested the evaluation of proposed vaginal pH as a good and inexpensive method. They reported that if vaginal pH>4.5, then serum estradiol is more likely to be the same as menopausal level.14
In the absence of vaginitis, a vaginal pH of 6-7.5 strongly suggests menopause.13–15 Health care providers suggest routine vaginal pH examination as a part of well-woman examinations and for diagnostic purposes in patients with symptoms of vaginitis or the request for hormone therapy.11 The purpose of this study is to compare serum follicle-stimulating hormone (FSH) level with vaginal pH in women with menopausal symptoms (according to the inclusion criteria, all the women had menopausal symptoms).
METHODS
This study is a cross-sectional descriptive study. The study subjects included 103 women with menopausal symptoms who were selected randomly from women referred to the Menopausal Clinic at Ghaem Hospital related to Mashhad University of Medical Sciences during 2006. A complete menstrual, sexual, medical and family history of early menopause was obtained and a questionnaire was completed for each woman including demographic characteristics (age, parity and body mass index), gynecological disorders and clinical manifestation of menopause. The patients’ age ranged between 31- 95 yrs.
The inclusion criteria specified women who had clinical symptoms of menopause (no menstrual bleeding for at least one year with exclusion of other causes of amenorrhea or FSH>20 mIU/ml). The exclusion criteria comprised of; pregnancy, vaginitis, hormone replacement therapy, and sexual intercourse within the previous three days. The protocol was approved by the Ethics Committee at Mashhad University and all the women gave an informed consent.
The two quantitative variants were serum FSH level and vaginal pH. Serum FSH level was measured using the Radio immunoassay (Wakerman, UK). All the women were referred to a specific laboratory where the results were given. Vaginal pH was measured using pH meter strip (Macherey nagel, Germany). During vaginal examinations, after the insertion of a non-lubricated sterile vaginal speculum, a 2 cm of the strip was applied directly to the lateral vaginal wall at the outer third of the vagina until it became wet. Color changes of the strip were immediately compared with the colorimetric scale and the measurements were recorded. The spaces between colors on the pH meter was 0.03, which was more accurate compared to conventional pH meters in which the spaces are 0.5 in pH unit. Care was taken to avoid cervical mucus or anything that may affect the vaginal pH.
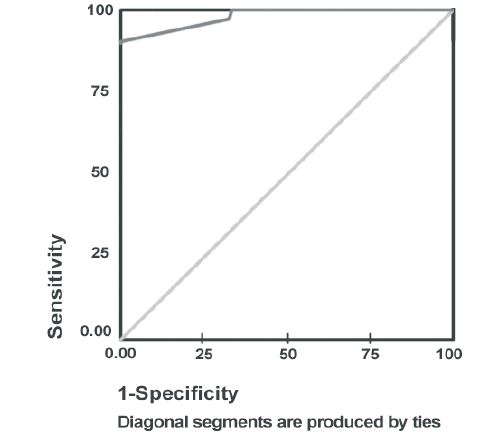
After data collection, statistical analysis was performed using SPSS software (version 11.5). Mc Nemar and Kappa tests were used to analyze the convergence of the two methods for the diagnosis of menopause. Moreover, Receiver operating characteristics (ROC) curve was used for the determination of cutoff point of pH with the highest sensitivity and specifity in regard to FSH test as a basic test. The Chi-square test was applied to compare different groups and p≤0.05 was considered statistically significant.
RESULTS
On the basis of the results from this study, the mean age of the patients was 54.28±8.59 yrs (ranging between 31-95 years) and 95% of the patients were below 70 years old. The length of amenorrhea was between 1 to 30 years. The mean and standard deviation for FSH level was 80.79±6.42 mIU/ml (ranging from 18.6 to 349 mIU/ml). The mean vaginal pH for the women was 5.33±0.53 (ranging from 4.1 to 5.9). According to this study, 97% of patients were determined to be menopausal on the basis of two criteria if FSH level was higher than 20 mIU/ml or if vaginal pH was ≥4.5 (all the women had menopausal symptom, but this test showed accurately that 97% of them were menopausal). In this study, by considering the FSH level as the base test and vaginal pH≥4.5 with the sensitivity of 97% and confidence limit of 100, 93.6 of the patients were menopausal (Table 1). Kappa and Mc Nemar tests also confirmed the convergence of the two methods (p=0.001).
Figure 1: ROC curve for determining the best cut off point in order to determine the highest sensitivity for vaginal pH test
DISCUSSION
Many menopausal women experience irregular menses and an array of symptoms long before they meet the definition of menopause.16 During menopause, two factors influence vaginal pH; menopausal status and the presence of potentially pathogenic organisms. In normal fertile women, lactobacilli maintain the normal acidic vaginal pH that protects the vagina against colonization.17 Some strains of lactobacilli produce hydrogen peroxide that prevents vaginal colonization with uropathogens.18 Therefore, the exclusion of vaginitis is essential for the vaginal pH to reflect the state of the menopausal vagina.
According to previous studies, there was a strong correlation between aging and increasing vaginal pH. During perimenopause, there is decreased number of functional follicles with less recruitment of oocytes upon FSH stimulation. Over time, as the aging follicles become more resistant to gonadotrophin stimulation, circulating FSH and leutinizing Hormone (LH) increase leading to stromal stimulation of the ovary, with an increase in estrogen and a decrease in estradiol levels. With the beginning of menopause and loss of follicles, the most significant change in the hormonal profile is the decrease in circulating estrogen levels.19 In menopausal women with urinary symptoms (such as dysuria) and raised vaginal pH, hormone replacement therapy can lead to normal vaginal pH and decreased symptoms.
In most postmenopausal patients who receive hormone replacement therapy, a vaginal pH of >4.5 may indicate low circulating levels of estradiol, which suggests the need for an adjustment of dose or route of hormone therapy. However, some patients with vaginal atrophy do not replenish their vaginal epithelium while receiving oral therapy, despite suitable circulating estradiol levels. For them, combining oral therapy with topical vaginal estrogen may be necessary. Atrophic vaginal epithelium permits greater absorption of estrogen compared with estrogenized epithelium.20 Some review articles indicated that serum FSH and vaginal pH have similar sensitivity in indentifying menopausal status.14
In a large epidemiologic study conducted in Costa Rica, vaginal pH was a functional index of aging and menopause.16 They reported that pH>5 has the sensitivity of 64-67% for the diagnosis of menopause.
In the current study, the sensitivity of vaginal pH in the diagnosis of menopause was 97%. Cailloutte et al. assessed vaginal pH and serum FSH level among 172 postmenopausal women. They reported that the sensitivity of vaginal pH in predicting estradiol status was 88%.13 Roy and colleagues reported that in the absence of vaginitis, a vaginal pH>4.5 indicated menopause with a sensitivity of 74%.11 The reported sensitivity of vaginal pH in the present study (97%) was more than the reported results in previous studies, perhaps because of the decrease in sexual activity or the decrease of intervention effect on vaginal pH.
Contradictory to the results from this study, Burger et al. reported that serum FSH was unsuitable to determine the presence menopause. They evaluated FSH levels among 150 women aged between 45-55 yrs for 6 years on the 4th and 8th day of every menstrual cycle and after three months of amenorrhea.21 In another study, Burger showed that both serum FSH and LH were of little diagnostic value in the assessment of menopause.6 Moreover, Gow et al. indicated that biochemical parameters do not guarantee menopausal status and cannot distinguish the early postmenopausal period from the period preceding menopause.22
In brief, according to this study, like serum FSH levels, vaginal pH is sensitive in the diagnosis of menopause, or low estrogenic status (97%).25 If vaginal pH is >4.5 in a menopausal woman, she can benefit from hormone therapy.24-25
CONCLUSION
In the absence of vaginitis, vaginal pH is a simple, accurate, and cost effective tool that can be suggested as a suitable alternative to serum FSH in diagnosing age-related hormonal changes. This method facilitates evaluation of the patient's baseline estrogen status and can be used for menopausal women to show the therapeutic efficacy and patient compliance with estrogen replacement therapy. However, further studies are required in appropriate design to evaluate the method of vaginal pH measurement for diagnosing menopause as a reliable and good replacement for FSH measurement.
ACKNOWLEDGEMENTS
The authors would like to thank Mrs Tooran Makhdoomi for editing this paper and Akram Moshtaghi that typed this collection. This article is the results of student thesis proposal of Dr. Gita Esfandyari.
-
Xu J, Bartoces M, Neale AV, Dailey RK, Northrup J, Schwartz KL. Natural history of menopause symptoms in primary care patients: A metronet study. J Am Board Fam Pract 2005; 18(15):374-382.
-
Cedars MI, Euans M, Scott JR, KarLan BY, Haney AF. Danforth 's obstertrics and gynecology . 9th .Philadelphia :Lippincott Williams and Wilkins. 2003: 721-739.
-
Soeriff KM, Frits MA. Clinical Gynecologic Endocrinology and in fertility 7th Edition. Philadelphia :Lippincott Williams & Wilkins Publishers . 2005; 621-640.
-
Mohammad K, Sadat Hashemi SM, Farahani FK. Age at natural menopause in Iran. Maturitas . 2004; 49(4):321-326.
-
Azzam AZ, AboulEinen WM, Karkour TA. Vaginal pH as a marker for the perimenopause: a comparison with follicle-stimulating hormone (FSH). Journal of the Medical Research Institute 2005; 26(3):273-278.
-
Burger HG. Diagnostic role of follicle-stimulating hormone (FSH) measurements during the menopausal transition – an analysis of FSH, estradiol and inhibin. Eur J Endocrinol 1994 Jan; 130(1):38-42.
-
Yoruk P, Uygur M, Erenus M, Eren F. The role of vaginal maturation value assessment in prediction of vaginal pH, serum FSH and E2 levels. Marmara Medical Journal. 2006;19(2):52-57.
-
Raz R, stamm WE. A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl Med 1993 Sep; 329(11):753-756.
-
Rein MF, Multer M. Trichomonas vaginalis and trichomoniasis. In: Holmes KK. Mard P-A, Spariling PF, Wiensner PJ, Cates JR, W, Lemon SM, et al . Sexually transmitted diseases 2th ed. New York: McGraw–Hill;1990:481-492.
-
Boskey ER, Telsch KM, Whaley KJ, Moench TR, Cone RA. Acid production by vaginal flora in vitro is consisitent with the rate and extent of vaginal acidification. Infect Immun 1999 Oct; 67(10):5170-5175.
-
Roy S, Caillouette JC, Roy T, Faden JS. Vaginal PH is similar to follicle-stimulating hormone for menopause diagnosis. Am J Obstet Gynecol 2004; 190(5):1272-1277.
-
Elia G, Bergman A. Estrogen effects on the urethra: beneficial effects in women with genuine stress incontinence. Obstet Gynecol Surv 1993 Jul; 48(7):509-517.
-
Caillouette JC, Sharp CF Jr, Zimmerman GJ, Ros S. Vaginal PH as a marker for bacterial pathogens and menopausal status. Am J Obstet Gyencol 1997 Jun; 176(6):1275-1277.
-
Milson I, Arvidsson L, Elrelund P, Molander U, Eriksson O. Factors influencing vaginal cytology, PH and bacteria flora in elderly women . Acta Obstet Gynecol Scand 1993 May; 72(4):286-291.
-
Pandit L, Ouslander JG. Postmenopausal vaginal atrophy and atrophic vaginitis. Am J Med Sci 1997; 314(4):228-231.
-
Garcia-Closas M, Herrero R, Bratti C, Hildesheim A, Sherman ME, Morera LA, et al. Epidemiologic determination of vaginal PH. Am J Obstet Gynecol 1999 May; 180(5):1060-1066.
-
Redondo-Lopez V, Cook RL, Sobel JD. Emerging role of lactobacilli in the control and maintenance of the vaginal bacterial microflora. Rev Infect Dis 1990 Sep-Oct; 12(5):856-872.
-
Kelbanoff SJ, Hillier SL, Eschenbach DA, Waltersdorph AM. Control of microbial flora of the vagina by H2O2 generating lactobacilli. J Infect Dis 1991 Jul; 164(1):94-100.
-
Smith KE, Judd HL. Menopause and postmenopause. In: Decherney AH, Pernoll ML, eds. Current Obstetric and Gynecologic Diagnosis and Treatment. 8th ed, Appleton and Lange, 1994; 1030-1050.
-
Melis GB, Ibba MT, Steri B, Kotsonis P, Matta V, Paoletti AM. Role of PH as a regulator of vaginal physiological environment. Minerva Ginecol 2000; 52(4):111-121.
-
Burger HD, Dudley EC, Hopper JL. Prospectively measured levels of serum follicle-stimulating hormone, estradiol and the dimeric inhibins during the menopause transition in a population-based cohort of women. J Clin Endocrinol Metab 1999 Nov; 84(11):4025-4030.
-
Gow SM, Turner EI, Glasier A. The clinical biochemistry of the menopause and hormone replacement therapy. Ann Clin Biochem 1994; 31:509-528.
-
Roy S, Caillouette JC, Faden JS, Roy T, Ramos DE. Improving appropriate use of antifungal medications: the role of an over-the counter vaginal Ph self-test device. Infect Dis Obstet Gynecol 2003; 11(4):209-216.
-
Casper F, Petri E. Local treatment of urogenital atrophy with an estradiolreleasing vaginal ring: a comparative and a placebocontrolled multicenter study. Vaginal Ring study Group. Int Urogynecol J Pelvic Floor Dysfunct 1999; 10(3):171-176.
-
Nilsson K, Risberg B, Heimer G. The vaginal epithelium in the postmenopause-cytology, histology and PH as methods of assessment. Maturitas 1995 Jan; 21(1):51-56.