Predictors of Positive Chest Radiography in Non‑Traumatic
Chest Pain in the Emergency Department
Nabil Al Zadjali,1 Rasha Al-Senawi,1 Abdullah Al Reesi,1 Ibrahim Al-Zakwani,2 Joe Nemeth,3 Jeffrey J. Perry 4
ABSTRACT
Objectives: To determine predictors associated with positive chest x-ray finding in patients presenting with non-traumatic chest pain in the Emergency Department (ED).
Methods: Health records, including the final radiology reports of all patients who presented with non-traumatic chest pain and had a chest x-ray performed in an urban Canadian tertiary care ED over four consecutive months were reviewed. Demographic and clinical variables were also extracted. Chest x-ray findings were categorized as normal (either normal or no significant change from previous x-rays) or abnormal. Descriptive statistics were used to describe the data. Multivariable logistic regression was used to determine the association between various predictors and chest x-ray finding (positive/negative).
Results: The 330 study patients had the following characteristics: mean age 58±20 years; female 41% (n=134). Patients’ chief complaints were only chest pain 75% (n=248), chest pain with shortness of breath 12% (n=41), chest pain with palpitation 4% (n=14), chest pain with other complaints 9% (n=28). Chest x-rays were reported as normal or no acute changes in 81% (n=266) of patients, and abnormal in 19% (n=64) of patients. The most common abnormal chest x-ray diagnoses were congestive heart failure (n=28; 8%) and pneumonia (n=17; 5%). Those with abnormal chest x-ray findings were significantly older (71 versus 55 years; p<0.001), had chest pain with shortness of breath (36% versus 11%; p<0.001), had significant past medical history (39% versus 14%; p<0.001), and were also tachypnoic (31% versus 12%; p<0.001).
Conclusion: This study found that patients with non-traumatic chest pain are likely to have a normal chest x-ray if they were young, not tachypnoeic or short of breath, and had no significant past medical history. A larger study is required to confirm these findings.
From the 1Department of Emergency Medicine SQU, Muscat, Oman, 2Department of Pharmacy, SQU, Muscat, Oman, 3Department of Emergency Medicine, McGill University, Montreal , QC, Canada, 4Department of Internal Medicine, University of Ottawa, Ottawa, ON, Canada.
Received: 29 Aug 2008
Accepted: 21 Nov 2008
Address correspondence and reprint request to: Dr. Rasha Al-Senawi, Department of Accident and Emergency, Sultan Qaboos University Hospital, 123 Al-Khod, Muscat, Sultanate of Oman.
E-mail: senawer@yahoo.com.INTRODUCTION
Radiology accounts for 6-10 % of all health care expenditures and chest radiography examination represents up to 50 % of the whole diagnostic radiology work‑up performed. It is a common tool used to evaluate patients in the Emergency Department (ED) with a wide variety of suspected chest and non-chest related complaints. Although this modality has been described as inexpensive, it is time consuming and potentially unnecessary in a large number of ED patients.1-5
Presently, chest radiography is a recommended initial screening test in traumatic patients as per the Advanced Trauma Life Support (ATLS) guidelines. In non-traumatic patients, plain film radiography reveals acute abnormalities in anywhere from 2.5 to 37% of ED patients selected to undergo chest x-ray.3,6-10 The low rate of positive films in most studies and the wide variability of significant abnormal films indicates there is a significant variation in clinical practice in the use of chest x-ray.11 This suggests that there is a potential for improved efficiency in current medical practice through the development of guidelines or a clinical decision rule.11
There has been a lot of confusion in the literature regarding the utility of chest radiography in an acute setting coupled with the lack of ED specific literature. Most previous studies of chest x-rays are confined to patients with asthma or chronic obstructive pulmonary disease (COPD) with varying recommendations. There have been few studies that have addressed the importance of chest radiography as a screening tool in non-emergency settings. In 1985, Hubbell et al. reviewed the literature on routine chest radiographs in internal medicine wards. They found that abnormalities were found in 36% of the patients but these findings resulted in treatment changes in only 4% of these patients. This study questions the value of indiscriminate use of chest x-rays. Another review of 997 ED asthmatics found that only 2.2% of adults had abnormal radiographs with all abnormalities occurring in those who had rhonchi or rales, or who were unresponsive to treatment.5 Based on their results, the authors did not recommend routine chest radiography in patients with asthma.2 Another review of 847 ED patients with COPD found that 16% had acute chest x-ray abnormalities with a quarter of these not predicted by previously developed high-yield criteria (prior congestive heart failure, coronary artery disease, peripheral edema, chest pain, or a white blood cell (WBC) count 15,000 cells/mm3.4,12 The authors of this study recommended routine chest radiography in all ED patients with COPD.4
Others have attempted to predict chest x-ray abnormalities in patients with non‑traumatic chest complaints and have been unable to develop sensitive criteria for predicting significant abnormalities.3,13 These studies did not address a focused clinical question. They attempted to predict abnormal chest x-ray findings in all the complaints (e.g. productive cough, fever, shortness of breath, palpitation, syncope, headache, traumatic chest pain) and not just patients with chest pain as in our study.
This study is attempting to define reasons behind non-traumatic chest complaints as well as factors associated with positive chest x-ray finding in an emergency room.
METHODS
Patient Population
This study was performed in the ED of an urban teaching hospital with an annual census of 75,000 in Canada. All patients presenting to the ED with chest pain between November 4, 2004 and February 28, 2005 and who underwent chest radiography were enrolled. Patients with a history of acute trauma and patients younger than 18 years of age were excluded. The institutional review board (IRB) approved this study without the need for informed patient consent as no change in patient management took place.
Data Collection
Health records were reviewed and patients identified from an ED computerized database. All patients (18 years and above) presenting with non-traumatic chest pain during the study period were enrolled into the study The standardized data extraction form for all patients included demographic data, their presenting symptoms to the ED, past medical history, vital signs, physical findings and a final discharge diagnosis. In addition, official radiologist reports were obtained for each of the patients who underwent chest radiography from the radiology database system (Magic web). Old radiographs were used by radiologists for comparison where available. Chest radiographs were defined as normal if this was the interpretation of the radiologist or if there were no new changes from previous imaging, despite a presence of non-significant findings. All other radiographs were defined as abnormal. We defined significant past medical history as the presence of COPD, cancer, asthma or congestive heart failure (CHF). All the data were extracted by one individual, the first author.
Statistical Analyses
Descriptive statistics were used to describe patient characteristics and clinical variables. For categorical variables, frequencies and percentages were reported. Differences between groups were analyzed using Pearson’s c2 tests (or Fishers Exact tests for cells less than five). For continuous variables, means and standard deviations (±SD) were presented. Mean differences between groups were analyzed using Student’s t‑tests.
A multivariate logistic regression analysis for the outcome of abnormal chest x-ray was conducted. The association of the following variables to an abnormal chest x-ray finding: age, chest pain type, past medical history, respiratory rate, last admitted location as the independent variables were determined. Independent variables were selected based on prior research.2-5 According to Peduzzi and colleagues,14 the useful rule of thumb from simulation studies is that for every parameter in the model, one needs at least ten outcomes. In this study, with the sample size of 330, of which 64 had positive chest x-ray finding, the ratio of positive outcomes to independent variables was approximately 10.7 to 1 (64/6), while the ratio of negative outcomes (n=340; 35%) to independent variables was approximately 44.3 to 1 (266/6). Both of the estimates are well within the recommended threshold. A priori two-tailed level of significance was set at the 0.05 level. Statistical analyses performed using STATA version 8.2 software.
RESULTS
A total of 330 patients were enrolled into the study. The demographic and clinical characteristics of the study cohort are shown in Table 1. Patients with positive chest x-ray findings were significantly older compared to those that had negative chest x-ray results (71 versus 55 years; p<0.001). They also had significantly higher proportion of subjects with chest pain and shortness of breath (SOB) or cough than other types of chest pain (36% versus 11%; p<0.001). The positive chest x-ray finding cohort had also higher percentage of patients with significant past medical history (39% versus 14%; p<0.001) and higher respiratory rate (>16 beats/minute) (31% versus 12%; p<0.001). Of note also was the fact that those with positive chest x-ray finding had higher proportion of subjects that ultimately required admission in ICU/CCU than with those that had negative chest x-ray finding (19% versus 6%; p=0.003).
Table 1: Demographic and clinical characteristics of the study cohort stratified by chest x-ray findings (N=330)
Characteristics |
Total (N=330) |
Chest X-Ray Finding |
P-value |
|
Negative (n=266) |
Positive (n=64) |
|||
Age, mean±SD*, years |
58±20 |
55±20 |
71±16 |
<0.001 |
Male gender, n (%) |
196 (59%) |
159 (60%) |
37 (58%) |
0.774 |
Chest pain type, n (%) |
|
|
|
|
Chest pain with SOB** or cough |
53 (16%) |
30 (11%) |
23 (36%) |
<0.001 |
All other types of chest pain |
277 (84%) |
236 (88%) |
41 (64%) |
|
Past medical history‡ (PMH), n (%) |
63 (19%) |
38 (14%) |
25 (39%) |
<0.001 |
Respiratory Rate (RR), n (%) |
|
|
|
|
Normal RR (12-16 /minute) |
279 (85%) |
235 (88%) |
44 (69%) |
<0.001 |
Heart Rate (HR), n (%) |
|
|
|
|
Normal HR (60-100 /minute) |
277 (84%) |
224 (84%) |
53 (83%) |
0.887 |
Low HR (<60 /minute) |
12 (3.6%) |
10 (3.8%) |
2 (3.1%) |
|
High HR (>100 /minute) |
41 (12%) |
32 (12%) |
9 (14%) |
|
Blood Pressure (BP), n (%) |
|
|
|
|
Normal BP (SBP*** 100-140 and DBP‡‡ 50-90 mmHg) |
219 (66%) |
175 (66%) |
44 (69%) |
0.396 |
High BP (SBP >140 or DBP >90 mmHg) |
102 (31%) |
85 (32%) |
17 (27%) |
|
Low BP (SBP <100 or DBP 50 mmHg) |
9 (2.7%) |
6 (2.3%) |
3 (4.7%) |
|
Oxygen saturation |
|
|
|
|
Normal saturation (≥95%) |
315 (95%) |
254 (95%) |
61 (95%) |
1.000 |
Respiratory examination, n (%) |
|
|
|
|
Normal |
283 (86%) |
230 (86%) |
53 (83%) |
0.522 |
Basal Crepitations |
15 (4.6%) |
11 (4.1%) |
4 (6.3%) |
|
Decrease Breath Sound |
12 (3.6%) |
10 (3.8%) |
2 (3.1%) |
|
Wheezing |
11 (3.3%) |
7 (2.6%) |
4 (6.3%) |
|
Bronchial Breathing |
9 (2.7%) |
8 (3.0%) |
1 (1.6%) |
|
Cardiovascular examination, n (%) |
|
|
|
|
Normal sound |
317 (96%) |
256 (96%) |
61 (95%) |
0.722 |
Last admitted location, n (%) |
|
|
|
|
Discharged home |
275 (83%) |
225 (85%) |
50 (78%) |
0.003 |
ICU/CCU |
28 (9%) |
16 (6%) |
12 (19%) |
|
Normal admission on regular ward |
27 (8%) |
25 (9%) |
2 (3%) |
|
*SD: Standard Deviation; **SOB: Shortness of Breath; ‡PMH was defined as the presence of either Chronic Obstructive Pulmonary Disease (COPD), Cancer, Asthma, or Congestive Heart Failure (CHF); ***SBP=Systolic Blood Pressure; ‡‡DBP=Diastolic Blood Pressure; ICU: Intensive Care Unit; CCU: Critical Care Unit; #P-values were generated using Student’s t‑tests, Pearson’s c2 test, and Fisher’s Exact test whenever appropriate. |
||||
The most frequent chief complaint was chest pain (n=248; 75%), followed distantly by chest pain with SOB (n=41; 12%), and chest pain with palpitation (n=14; 4%). Other presenting complaints are listed on Table 2. Despite the fact that all the subjects had chest pain, the majority (n=266; 80.6%) had normal chest x-ray finding.
Table 2: Chief complaint stratified by Negative and Positive Chest Findings (N=330)
Diagnosis |
Chest Finding |
Total (%) |
|
Negative (n=266) |
Positive (n=64) |
||
Plain Chest Pain (CP) |
213 |
35 |
248 (75%) |
CP with Shortness of Breath |
22 |
19 |
41 (12%) |
CP with Cough |
8 |
4 |
12 (3.6%) |
CP with Fever |
3 |
1 |
4 (1.2%) |
CP with Palpitation |
12 |
2 |
14 (4.2%) |
CP with Syncope |
5 |
1 |
6 (1.8%) |
CP with Weakness |
0 |
1 |
1 (0.3%) |
CP with Epigastric Pain |
2 |
1 |
3 (0.9%) |
CP with Miscellaneous |
1 |
0 |
1 (0.3%) |
CP: Chest Pain |
|||
Table 3 showed the most frequent diagnoses stratified by the positive and negative chest x-rays. The most frequent preliminary diagnoses were CHF (n=28; 8%) and pneumonia (n=17; 5%).
Table 3: Final diagnoses stratified by Negative and Positive chest findings (N=330)
Diagnosis |
Chest Finding |
Total (%) |
|
Negative (n=266) |
Positive (n=64) |
||
Normal |
251 |
0 |
251 (76%) |
Pneumonia |
0 |
17 |
17 (5.2%) |
Congestive Heart Failure |
0 |
28 |
28 (8.5%) |
Pleural Effusion |
0 |
11 |
11 (3.3%) |
Cancer |
0 |
6 |
6 (1.8%) |
Pulmonary Embolism |
0 |
2 |
2 (0.6%) |
Miscellaneous |
15 |
0 |
15 (4.6%) |
Figure 1 outlines the probability of a positive chest x-ray finding while varying age, generated using multivariable logistic regression. The figure clearly demonstrates that the association is positive. The probability of a positive chest x-ray result increased with age. The graph also indicates that those with chest pain and SOB (or cough), significant past medical history, and higher respiratory rate had clinically significantly higher probability of a positive chest x-ray finding than those with other types of chest pain, insignificant past medical history, and normal respiratory rate. Even at the minimum age of the cohort, the probability of having a positive chest x-ray result was already nearly four times higher for those with chest pain and SOB (or cough), significant past medical history, and higher respiratory rate compared to their counterparts.
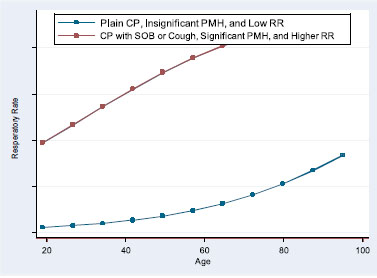
Figure 1: A graph of the probability of a positive chest x-ray finding while varying age generated using multivariable logistic regression (N=330).
DISCUSSION
This was the first study, which looked at patients with non-traumatic chest pain who presented to the ED as well as determining various factors that could potentially predict abnormal chest x-ray findings. Among the chief complaints observed were chest pain only, chest pain with shortness of breath, and chest pain with palpitation. Only 19% of all non-traumatic chest x-rays were positive. The study also demonstrated that a positive chest x-ray finding was associated with those who were older, had chest pain with shortness of breath, significant past medical history, and those who were tachypnoeic.
Unexpectedly, this study noted that reduced air entry, rhonchi or crackles were not predictive variables although previous studies have showed this to the contrary. This could be due to either inappropriate documentation of findings in a very busy ED and/or due to the smaller number of patients in our cohort.
By using the multivariable logistic regression model, this study also found that patients’ age is one of the important predictors to increase the probability of having significant chest x-ray abnormalities. Two groups of patients could be deduced from this study with regards to chest x-ray finding. High-risk group are those patients who presented to the ED with chest pain associated with cough, SOB, significant past medical history (COPD, cancer, asthma or CHF) or high respiratory rate. On the other hand, the low-risk patients are those who presented to the ED with chest pain but with no significant past medical history or with low respiratory rate. Age over 65 years, in the low-risk group, was associated with 15% probability of having a significant finding on chest x-ray, and the probability of a positive chest x-ray result was increasing with age thereafter. However, in the high-risk group, significant chest x-ray abnormalities were found even in younger age groups, and the probability increased dramatically as age increased (Figure 1).
This study was conducted at a single center, which is affiliated to an Emergency Medicine Residency Training Program. While this was a large, busy ED, the results of this study should be validated in other centers to confirm our findings. It can be argued that the physical examination assessment is performed by the training residents. Their findings may differ from one resident to another depending on their training level, which could have affected the findings. Unfortunately, we could not calculate the kappa to compare the degree of agreement between the residents and the emergency department staff because of inadequate information in the Magic-Web database. In addition, this was a retrospective study, so there was no uniform definition of historical key features as well as a standardization of the physical examination findings. The character of the chest pain was not included in the study, which could have led to different working strategy of patients. The findings should be interpreted in light of the present limitations.
CONCLUSION
Our study of an urban tertiary care ED found that patients with chest pain are likely to have a normal chest x-ray if they were young, not tachypnoeic or short of breath, and had no significant past medical history. This could lead to reduction in unnecessary chest x-ray requests in the ED in such patients and could potentially lead to a shorter patient stay in the ED. A larger prospective study is required to confirm these findings.
ACKNOWLEDGMENTS
The authors report no conflict of interest and no funding has been received in this work.
-
Buenger RE. Five thousand acute care/emergency department chest radiographs: comparison of requisitions with radiographic findings. J Emerg Med. 1988; 6:197-202.
-
Russell NJ. The role of chest radiography in patients presenting with anterior chest pain to the Accident & Emergency Department. J R Soc Med. 1988; 81:626-628.
-
Rothrock SG. High yield criteria for obtaining non-trauma chest radiography in the adult emergency department population. J Emerg. Med. 2002 Jan; Vol 23, No. 2, pp. 117-124.
-
Clinton JE, Yaron M, Tsai SH. Chest radiography in the emergency department. Ann Emerg Med 1986; 15:254-256.
-
Aronson S, Gennis P, Kelly D, Landis R, Gallagher J. The value of routine admission chest radiographs in adult asthmatics. Ann Emerg Med 1989; 18:1206-1208.
-
Diehr P, Wood RW, Bushyhead J. Prediction of pneumonia in outpatients with acute cough-a statistical approach. J Chron Dis 1984; 37:2215-2225.
-
Emermann CL, Cydulka RK. Evaluation of high-yield criteria for chest radiography in acute exacerbation of chronic obstructive pulmonary disease. Ann Emerg Med 1993; 22:680-684.
-
Zieverink SE, Harper AP, Holden RW, Klatte EC, Brittain H. Emergency room radiography of asthma: an efficacy study. Radiology 1982; 145:27-29.
-
Benacerraf BR, McLoud TC, Rhea JT, Tritschler V, Libby P. An assessment of the contribution of chest radiography in outpatients with acute chest complaints: a prospective study. Radiology 1981; 138:293-299.
-
Russell NJ, Pantin CF, Emerson PA, Crichton. The role of chest radiography in patients presenting with anterior chest pain to the Accident and Emergency Departments. J Royal Soc Med 1988; 4:383.
-
Sherman S, Skoney JA, Ravikrishnan KP. Routine chest radio-graphs in exacerbations of chronic obstructive pulmonary disease: diagnostic value. Arch Intern Med 1989; 149:2493-2496.
-
Landis RJ, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33:159-174.
-
Noeller TP, Bessleer R, Meldon SW, et al. Does a normal physical exam preclude the need for chest radiographs in ED patients with non-traumatic chest pain? (abstract) Acad Emerg Med 1998; 6:541-542.
-
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 1996; 49:1373-1379.