Photodynamic Therapy with Verteporfin for Chronic Central Serous Choroidoretinopathy and Idiopathic Choroidal Neovascularization- First Report from the Sultanate of Oman
Upender Krishen Wali, Nadia Al-Kharousi, Harith Hamood
ABSTRACT
Background: Central Serous Chorioretinopathy (CSCR) is characterized by accumulation of subretinal fluid, resulting in neurosensory retinal detachment.
Design: Interventional study.
Methods: Five patients (CSCR-3; Idiopathic-2) with Choroidal Neovascularization (CNV) were selected for the study. All patients had Standardized refraction, color photographs, fluorescein angiography (FA), and Photodynamic Therapy (PDT) using verteporfin. Optical Coherence Tomography (OCT) was done wherever applicable. The main outcome measures were improvement or stability in Best Corrected Visual Acuity (BCVA) and FA identified closure of lesions.
Results: Followup period for the CSCR group ranged from 8 to 11 months and for the idiopathic group 12 to 23 months. BCVA improved in 67% eyes in the CSCR group (three eyes). Amongst the idiopathic group (two eyes), one eye gained BCVA by two lines while the other lost one Snellen line from baseline VA. FA identified CNV lesions closed in 67% eyes in the CSCR group and all eyes in the idiopathic CNV group.
Conclusions: Photodynamic therapy with Verteporfin can be an ideal mode of therapy in chronic CSCR with or without CNV, and idiopathic CNV in terms of improved or stabilized VA, and closure of the CNV lesions. A study involving a larger number of patients as a multicenter trial would add to the authenticity of our observation.
Keywords: Central Serous Chorioretinopathy, verteporfin
Submitted : 07 Aug 2008
Reviewed: 23 Aug 2008
Accepted: 19 Sept 2008
From the Department of Ophthalmology, Sultan Qaboos University, College of Medicine and Health Sciences, Muscat, Oman.
Address correspondence and reprint requests to: Dr. Nadia Al Kharousi, Department of Ophthalmology, Sultan Qaboos University, College of Medicine and Health Sciences, Al Khoud 38, Muscat, Oman ZIP 123.
E-mail: nadiqi@hotmail.com
INTRODUCTION
Neonatal Central Serous Choroidoretinopathy (CSCR) is characterized by accumulation of subretinal fluid at the level of the retinal pigment epithelium, resulting in a circumscribed neurosensory retinal detachment.1 Patients usually present with metamorphopsia and moderately reduced visual acuity (VA). CSCR typically affects young and middle-aged males.2 In most cases, CSCR resolves within a few months and VA returns to normal. However, in a few patients, as reported in our study, the disease takes a chronic course and the RPE alterations, metamorphopsia persist.1,2 Occasionally choroidal neovascularization (CNV) develops in chronic CSR when intervention with laser is indicated.3
We report three patients with chronic CSCR and two patients with idiopathic CNV who underwent PDT therapy with verteporfin, and showed significant improvement in terms of best corrected visual acuity (BCVA) and closure of fundus fluorescein angiography (FA) identified CNV lesions. The minimum and maximum duration of CSCR in our study was 8 months and 23 months respectively. The purpose of this study is to evaluate the outcome of visual acuity and CNV lesions after photodynamic therapy in CSCR and idiopathic choroidal neovascularization.
METHODS
Settings: This institutional interventional noncomparative study comprised five consecutive patients (five eyes; CSCR - three, idiopathic-two) undergoing verteporfin PDT therapy at the university hospital, Oman between 2004 and 2007. The indications for the therapy included juxtafoveal CNV (one each from the CSCR and idiopathic group), one extrafoveal CNV in the idiopathic group, and two chronic CSCR lesions without choroidal neovascularization, which did not resolve even after a minimum eight months of natural course.
The control group would have been those patients left untreated which was not possible in our study due to the small number of patients.
The inclusion criteria were: (1) Fundus fluorescein angiography (FA) identified leaking CNV lesions. (2) Nonresolving CSCR with decrease in VA and persisting metamorphopsia.
Exclusion criteria were: (1) Eyes having had previous laser, surgery, anti-VEGF therapy, inflammations, and retinal vascular diseases. (2) Pregnancy.
The study was performed in accordance with the Declaration of Helsinki protocol. Written informed consent was obtained from all patients. Approval of the institutional ethics committee (MREC) was not necessary. A minimum followup period of six weeks was decided. Patients underwent a complete eye examination at baseline and each visit in the followup, not exceeding seven days before PDT. The examination included BCVA with Snellen charts (10‑step charts) at six meters, slit-lamp biomicroscopy (Haag-Streit, Switzerland), funduscopy, color fundus photography and FA (ImageNet Topcon). OCT (Zeiss II) was done wherever applicable. FA images of each eye were analyzed by two observers (NK, UW). Wherever doubt existed, opinion of a third, masked observer, not involved in the study, was taken. FA was done a maximum of two weeks, minimum of 72 hours before treatment, and 12 weeks after each PDT treatment in the majority of cases. The FA interpretation of CNV lesions was done using the guidelines of the Macular Photocoagulation Study (MPS) group.4 The size of the lesions was measured in disc areas. The patients were reviewed at six to 12-week intervals. The aim of the study was to follow up for two years. To assess treatment effects, we analyzed the number of Snellen lines gained, unchanged or lost at each visit. The date of the first treatment was used for analysis.
Verteporfin PDT (Visudyne; Novartis AG, Switzerland) was performed under standard treatment protocol using a single spot of light that covered 1000 microns larger than the greatest linear dimension of CNV lesion as determined by digital angiography (ImageNet Topcon).5
Table 1: Patients and Results
Patient no. |
Age (year) |
Gender |
Diagnosis |
Follow up (months) |
BCVA baseline |
BCVA final |
BCVA gain/loss |
CNV lesion size |
CNV lesion type |
Number of PDTs |
1 |
33 |
F |
CSCR |
11 |
6/6 |
6/6 |
± |
none |
|
1 |
2 |
50 |
M |
CSCR |
8 |
6/15 |
6/9 |
+ 2 |
0.76DD |
juxtafoveal |
1 |
3 |
40 |
M |
CSCR |
11 |
6/60 |
6/18 |
+5 |
none |
|
1 |
4 |
42 |
F |
Idiopathic |
12 |
6/9 |
6/6 |
+2 |
1.07DD |
juxtafoveal |
1 |
5 |
20 |
F |
Idiopathic |
23 |
6/15 |
6/18 |
-1 |
1.23DD |
extrafoveal |
1 |
F=Female, M=Male, CSCR=Chronic Central Serous Choroidoretinopathy, ± = No change in Best Corrected Visual Acuity (BCVA), +=gain in BCVA, - = Loss in BCVA, CNVC= Choroidal neovascularization, DD= Disc diameters, PDT=Photodynamic therapy. |
||||||||||
RESULTS
Five patients (five eyes: three with chronic CSCR, and two with idiopathic CNV) underwent photodynamic therapy using verteporfin. These included two (40%) males and three (60%) females (CSCR: M-2: F-1; Idiopathic: F-2). Each patient had one PDT treatment only. The age for CSCR group ranged from 33 years to 55 years (mean = 41 years) and for the idiopathic group 20 years to 42 years (mean = 31 years). Mean followup period until completing this part of the study was 10 months (range, 8 – 11 months) for the CSCR group and 17.5 months (range, 12 – 23 months) for the idiopathic group. Baseline (Pre-PDT) Snellen BCVA ranged from 6/6 to 6/60 (mean 6/12) for the CSCR group and 6/9 to 6/15 (mean 6/12) for the idiopathic group. The distribution of the location of CNV was as follows:
CSCR group: juxtafoveal (1 eye). Patient 2; Fig-1
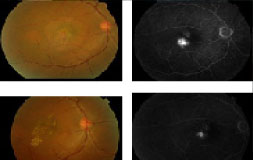
Figure 1: Patient 2. OD:
Figure 1. Patient 2. Chronic Central Serous Choroidoretinopathy (CSCR).
OD: Top left: Classic chronic CSR at first presentation. Top right: FA identified juxtafoveal leaking Choroidal neovascularization (CNV). Bottom left: Three months after first PDT the CSCR showed significant resolution. Bottom right: FA identified smaller than before and less intense leakage. Second PDT was withheld due to RPE detachment after first PDT. Eight months after only PDT, BCVA improved from 6/15 to 6/9.
Idiopathic group: juxtafoveal (1 eye) Patient 4; Fig 3 extrafoveal (1 eye).
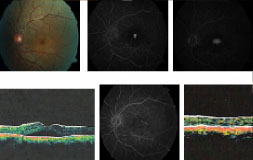
Figure 2: Patient 3. OS
Figure 2. Patient 3. Classic chronic Central Serous Choroidoretinopathy.
OS: Top left: Pre PDT color image, and FA (top center and top right) showing classic CSCR. Bottom left: OCT (central 1.0mm) before PDT showed retinal thickness of 342 microns with subretinal fluid. After first PDT, patient had almost complete resolution of subretinal fluid with residual exudates (bottom center) and OCT documented resolving subretinal fluid (bottom right, thickness 201 microns). His BCVA improved from 6/60 to 6/18 three months after PDT.

Figure 3: Patient 4. OS
Figure 3. Patient 4: Juxtafoveal CNV.
OS: Top left: color image. Clinical diagnosis: Idiopathic CNV. Top right: FA identified early leakage. Bottom left: late leakage. Bottom right: FA identified closure of CNV with residual staining 4 months after only PDT. Patient’s final BCVA was 6/6.
The mean CNV lesion size (greatest linear dimension) measured 1.15 DD (range, 1.07–1.23 DD) for the idiopathic group. The only CNV lesion in one eye in the CSCR group measured 0.76 DD. FA identified CNV lesions had closed in all three eyes (two idiopathic, Fig 3 and one CSCR, (Fig 1) at the time of last follow. Amongst the CSCR group without CNV (two eyes), one eye had almost completely resolution (Fig 2).
However, the other eye developed RPE detachment after PDT which resolved conservatively with final BCVA of 6/6. Patients in the CSCR group showed mean improvement of 3.5 lines (range 2–5 lines; mean post PDT BCVA 6/9) in 67% eyes, one eye (33%) had no change in BCVA from the baseline. From the idiopathic group, one eye improved by two lines while other lost one line from the baseline BCVA (mean post PDT BCVA 6/9).
Overall in both groups, all except one eye showed improved or stable vision, and improvement in metamorphopsia at the end of mean follow up of 13.7 months.
DISCUSSION
Though steroids, pregnancy, Cushing’s syndrome, systemic hypertension, lupus erythematosus have been implicated in the pathogenesis of CSCR, it is not known whether any of these conditions predisposes to CNV or not. The condition has been reported to be occasionally familial.6-11 A recent study has identified new risk factors such as antibiotic and alcohol use and allergic respiratory disease.12 We could not identify the etiology for CNV in two patients, hence they were put in the idiopathic group. The laser treatment of CSCR remains a controversial issue because of the favorable visual outcome after spontaneous remission of the disease. However, this may not be always true in chronic cases of CSCR where symptoms persist for months or years and intervention may be justified.3 Also, persistent detachment of fovea in chronic CSCR may lead to atrophic degeneration of the retina and RPE, with no scope of improvement of vision even after resolution of the detachment. Since laser photocoagulation is associated with permanent scotomata, RPE scarring, and possible choroidal neovascularization, PDT may be an ideal choice in chronic CSCR.13
Verteporfin accumulates in RPE cells due to their high lipid content and the drug binds to low-density lipoprotein receptors on endothelial cells. The direct action of PDT on choriocapillaris endothelium produces occlusion and reduced vascular permeability. RPE cells damaged by PDT are replaced by new ones with normal anatomical, physiologic and metabolic functions.14 All our CSCR patients had improvement or stable VA after PDT. OCT (patient 3) confirmed the resolution of subretinal fluid (Fig 2), and FA identified closure of leakage (Fig 2). OCT documented reduction in subretinal fluid, improved vision, and stoppage of leakage has been reported by Mehryar T et al.15
Michael D. Ober et al. in a series of nine eyes with chronic CSCR reported resolution of neurosensory detachment and leakage in all patients, as has been observed in our three patients as well.16 The VA in Ober’s study improved in 77% patients (seven eyes), compared to 67% (three eyes) in our study. One (patient 2) of our three CSCR patients had CNV which showed decrease in size as well as intensity of leakage of the lesion three months after PDT (Fig 1).
CONCLUSION
This study, though marked by limitations such as absence of control group and small number of patients, showed convincing results in terms of VA output, amelioration of symptoms, closure of CNV, and resolution of subretinal fluid. Also, the results are compatible with other studies related to PDT in chronic CSCR. We think there have been three outcomes of this study:
1. PDT is definitely a treatment of choice in symptomatic chronic CSCR as well as idiopathic CNV.
2. PDT-related complications such as RPE detachment can resolve completely with no deficit in VA.
3. Studies involving a larger number of patients are required for better understanding of the role of PDT in chronic CSCR and idiopathic CNV.
ACKNOWLEDGEMENT/DISCLOSURE
a) Funding: The authors have no commercial or proprietary interest in any of the instruments or drugs mentioned in the study. No financial support / funding has been received from any source during this study.
b) Financial disclosure: see attachments for three authors.
c) Authors contribution: see attachment.
d) The medical research ethics committee of Sultan Qaboos University waived the need for approval on the basis that photodynamic therapy is an accomplished and FDA approved method of treatment. However, informed and written consent was taken from all patients before the treatment.
The study was performed in accordance with the Declaration of Helsinki protocol.
e) No statistical evaluation was done due to small sample size.
-
J.D.M. Gass. Stereoscopic atlas of macular diseases; diagnosis and treatment. CV Mosby Co. 4th ed. St Louis 1997; p. 52-70.
-
Klein ML, Van Buskirk EM, Friedman E, Gragoudas E, Chandra S, et al. Experience with nontreatment of central serous choroidopathy. Arch Ophthalmol 1974; 91:247-250.
-
Hussain D, Gass JD. Idiopathic chronic central serous chorioretinopathy. Indian J Ophthalmol 1998; 46:131-137.
-
Friberg TR, Eller AW. Serous retinal detachment resembling central serous chorioretinopathy following organ transplantation. Graefes Arch Clin Exp Ophthalmol 1990; 228:305-309.
-
Matsuo T, Nakayama T, Koyama T, Matsuo M. Multifocal pigment epithelial damages with serous retinal detachment in systemic lupus erythematosus. Ophthalmologica 1987; 195:97-102.
-
Macular Photocoagulation Study Group. Subfoveal neovascular lesions in age-related macular degeneration: guidelines for evaluation and treatment in the macular photocoagulation study. Arch Ophthalmol 1991; 131:541-560.
-
Verteporfin in Photodynamic Therapy (VIP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in pathological myopia with verteporfin: Ophthalmology 2001; 108:841-852.
-
Yannuzzi LA, Slakter JS, Gross NE, Spaide RF, Costa DL, Huang SJ, et al. Indocyanine green angiography guided photodynamic therapy for treatment of chronic central serous chorioretinopathy: a pilot study. Retina 2003; 23:288-298.
-
Spaide RF, Martin ML, Slakter J, Yannuzzi LA, Sorenson J, Guyer DR, et al. Treatment of idiopathic subfoveal choroidal neovascular lesions using photodynamic therapy with verteporfin. Am J Ophthalmol 2002; 134:62-68.
-
Loo JL, Lee SY, Ang CL. Can long-term corticosteriods lead to blindness? A Case Series of Central Serous Chorioretinopathy Induced by Corticosteroids. Ann Acad Med Singapore 2006; 35:496-499.
-
Bedrossian RH. Central serous retinopathy and pregnancy [letter]. Am J Ophthalmol 1974; 78:152.
-
Bouzas EA, Scott MH, Mastorakoss G, et al. Central serous chorioretinopathy in endogenous hypercortisolism. Arch Ophthalmol 1993; 111:1229-1233.
-
Haik GM, Perez LF, Murtagh JJ. Central serous retinopathy. Consecutive development in daughter and mother. Am J Ophthalmol 1968; 65:612-615.
-
Haimovici R, Koh S, Gagnon DR, Lehrfeld T, Wellik S, Central Serous Chorioretinopathy Case-Control Study Group. Risk Factors for Central Serous Chorioretinopathy A Case–Control Study. Ophthalmology 2004; 111: 244–249.
-
Mehryar T, et al. Chronic central serous chorioretinopathy: photodynamic therapy. American Journal of Ophthalmology 2004; 137:1073-1080.
-
Robertson DM. Argon Laser Photocoagulation treatment in central serous chorioretinopathy. Ophthalmology 1986; 93:972-974.
-
Parodi MB, Pozzo SDA, Ravalico G. Photodynamic therapy in chronic central serous choroidopathy. Retina 2003; 23:235-237.
-
Michael D. Ober, Lawrence A. Yanuzzi, Do DV. Photodynamic therapy for focal retinal pigment epithelial leaks secondary to central serous chorioretinopathy. Ophthalmology 2005; 112:2088-2094.