|
Abstract
Objectives: This study estimated the merit of employment of Grading Fine Needle Aspiration Cytology (GFNAC) in the assessment of breast lumps, compared to conventional Conventional Fine Needle Aspiration Cytology (CFNAC).
Methods: Seventy-five women with breast lumps were referred to the surgical unit at Khartoum Teaching Hospital. Fine Needle Aspiration (FNA) materials were obtained for cytology and biopsies from the same patients for histopathology. Cytological materials were assessed using two diagnostic systems (GFNAC and CFNAC) without prior knowledge of the histopathologic diagnosis.
Results: Of the 75 patients studied, 40 (53.3%) were diagnosed as having breast cancer by Histopathology and the remaining 35 (46.7%) were diagnosed with benign lesions. Of the 40 positive cases, 35 (87.5%) and 28 (70%) were found positive by CFNAC and GFNAC respectively. Of the 35 negative cases, 33 (94.3%) and 35(100%) were found negative by CFAC and GFAC correspondingly.
Conclusion: The obtained Specificity of 94.3% and 100% in addition to sensitivity of 87.5%, 70% were credited for CFNAC and GFNAC systems respectively. Therefore, it is recommended to merge GFNAC as a supplementary to CFNAC for the diagnosis of breast cancer.
Introduction
Fine-needle aspiration cytology (FNAC), as practiced today is an interpretive art with histopathology as its scientific base.1 FNAC is a simple and less traumatic diagnostic technique which offers many advantages both to the patient and surgeon. FNAC of the breast has been shown to be a safe and accurate technique, although many surgeons question whether it is reliable enough to replace excisional biopsy. If FNA is followed by excisional biopsy for confirmation, it would seem that the cost of diagnostic work-up would be increased. However, the major economic benefit of FNA is not that it replaces excisional biopsy, but that it allows the surgeon to decide which patients should have FNA or excisional biopsy.2 FNAC has an average sensitivity of 87%, specificity of 99%.3 A problem inherent to this technique is to obtain an insufficient specimen.4
Female breast cancer is by far the leading cancer in the Sudan, which has been recognized as an important health problem, which is associated with a high rate of mortality and morbidity. The highest percentages were recorded in 1998 (38.4%) of all female cancers (as reported by Radiation Isotope Center Khartoum).5
On the other hand, most of these cases present with late stages of the disease. In view of that, the implementation of simple, less invasive and inexpensive dealings is important for early detection and planning for an appropriate treatment of the disease. Clinical examination and mammography alone or together do not identify all malignant breast lesions. Because of this, in order not to miss malignancy, all solid breast lesions require microscopic diagnosis. Open biopsy is the most sensitive diagnostic technique, but it is less desirable because approximately 20-25% of clinically suspicious prove to be malignant on histology.3 This means that about 75% of the biopsies performed for benign lesions.
Therefore, the application of less invasive, quick and cheap technique is very consequential, particularly in a country like the Sudan, where many patients present from remote areas with poor health services. For that reason, the incidence and mortality of breast cancer are high, remarkably constant and the frequency is increasing, particularly amongst younger women.
This study evaluated the possibility of introducing a new system (GFNAC) for the diagnosis of palpable breast lumps, as a preoperative diagnostic tool, and to compare it to CFNAC. The findings of this new system (GFNAC) were compared to histopathology of the gold standard.
Methods
Seventy-five patients with breast masses were selected depending on the clinical suspicious. All subjects were females of 20 years of age or older. A questionnaire to obtain essential data about each patient was used. Two specimens were collected from each patient:
a) FNA- where Breast aspiration was made by surgeon in charge and cytologist. The palpable lumps were aspirated using 10 ml disposable syringe. Material was expressed onto glass slides and smeared. The smear was immediately fixed in 95% alcohol while it was wet, then stained adopting the Papanicolaou (Pap.) staining method.6
b) Biopsy- where each biopsy (excisional or diagnostic) that has been sent by the surgeon to the laboratory for histopathology was directly placed in 10% neutral buffered formalin. Sections of 5µm in thickness were obtained from formalin-fixed paraffin wax embedded tissue blocks using a Rotary microtome. Sections were stained using Hematoxylin and Eosin staining methods adopting Mayer's Procedure.6
All cytological smears were investigated adopting two examination systems (CFNAC to detect malignant features and GFNAC to assess the degree of cytological atypia). The criteria for the ascertainment and assessment of the degree of cytological atypia were adopted from those previously reported by Ahmed et al. (2003).7 The criteria of atypia included the presence of the major malignant features including; nuclear enlargement associated with increased nuclear cytoplasmic ratio, hyperchromatism, chromatin clumping with moderately prominent nucleolation and irregular nuclear borders, bi or multinuclation, and scantiness of the cytoplasm and variations in size and/or shape of the cells and nuclei.
Three possible grades are provided for each of the characteristics. The first of these allows for the fact that the characteristic may be absent completely (i.e. "None") or present in its normal form (i.e. "Normal"). The other two grades allow for different degrees of severity and were assessed by comparison with each of the photographs which illustrate the grade of atypia (slight or marked) as shown elsewhere.8,9 For scoring during the examination of the smears, one grade (only one) was chosen for each characteristic according to the comparison with the appropriate photograph illustrated elsewhere.10
The formula below was used to obtain the percentage of cells showing atypia. Both normal cells and cells showing features of cytological atypia were counted in 5 microscopical fields using a magnification of an objective lens of 40X, and the mean of the count was then calculated for both types of cells. The two means were added together, and the total mean of cell count per field was obtained. According to the counts above, the percentage was obtained using this equation:
% of cells showing atypia = The mean of abnormal cells/ field X 100
The total mean of cells/field
If only one atypical characteristic is apparent in 3-15% of the cells, the grade is considered as slight, and are further given the following score values for each one characteristic: (+) for 3-6% atypical cells; (++) for 7-10% atypical cells; and (+++) for 11- 15% atypical cells. The score value (+++) is comparable to marked changes scoring (+), which is equal to mild cytological atypia.
If two or more characteristics appear or the one characteristic appears in more than 15% of the cells the grade is considered as marked, and the score value is given as follows:
a) If atypical feature for one characteristic was found in 16-20% of the cells, the scoring is assigned (+), which is equal to mild cytological atypia, b) In 21-50% of atypical cells, the scoring is assigned (++), which is equal to moderate cytological atypia, and c) In over 51% of cells atypia, the scoring is assigned (+++), which is often showing severe cytological atypia.
No cytological atypia was considered unless the slight features scored (+++). Scores of different characteristics were eventually gathered to identify the degree of atypia. One of three degrees of cytological atypia was reported; mild, moderate or severe. Severe cytological atypia is equal to malignancy.
Each participant was asked to sign a written ethical consent during the interview, before the specimen was taken. All specimens were taken as part of the specimens required for diagnosis. The informed ethical consent form was designed and passed by the ethical committee of the Faculty of Medical Laboratory Research Board, University of Khartoum.
Results
As histopathology is a gold standard, two independent examiners histopathologically investigated sections from 75 patients with breast lesions, their age ranging from 20 to 75 years with a mean age of 40 years. Forty patients were reported as having breast cancer by two investigators and the remaining 35 were diagnosed with different benign conditions.
Results of histopathology were used as a gold standard to evaluate the results obtained by CFNAC or GFNAC. Of the 40 positive specimens (diagnosed as having breast cancer) by histopathology, 35 (87.5%) were found positive by CFNAC, hence the remaining five (12.5%) were found to be negative. Of the 35 negative specimens (patients diagnosed as having benign breast tumors) by histopathology; 33 (94.3%) were found negative by CFNAC and the remaining two (5.7%) were identified as negative (diagnosed with malignant changes). (Figs. 1, 2)
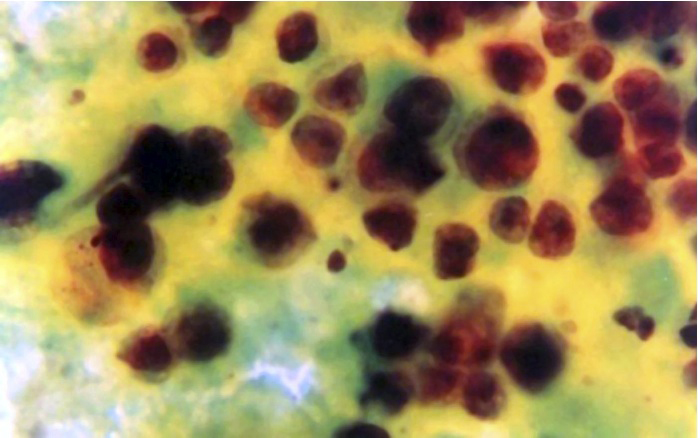
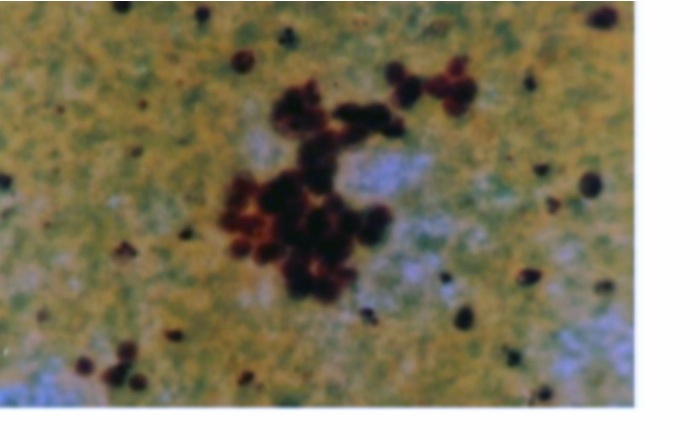
Figure 1: Ductal carcinoma of the breast: The smear is cellular, cell are dissociated and overlapping, nusclear cytoplasmic ration is high, nuclei are hyperchromatic (Papaniclaoustain, A.X200 and B.X400).
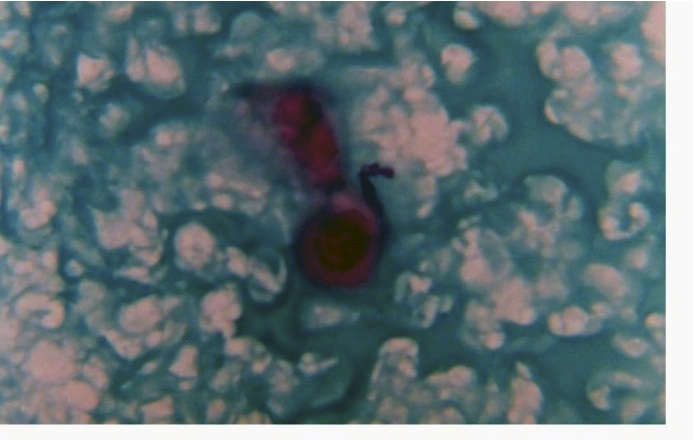
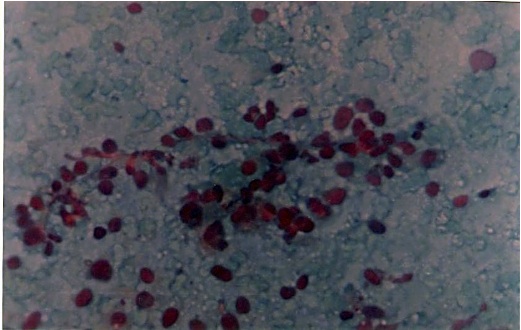
Figure 2: FNA of the breast: severely altered galactophoruos cells surrounded by a clearly hemorrhagic background substance. The smear is corresponding to an Intraductal Carcinom (Papaniclaoustain, A.X200 and B.X400).
With regard to GFNAC, of the 40 positive specimens by histopathology, 28 (70%) were detected with severe cytological atypia (corresponding to malignant change) by GFNAC, and the remaining 12 (30%) were found to be negative. The negative smears by GFNAC were further categorized as: two (5%) showing moderate atypia (parallel to suspicious), three (7.5%) characterizing mild atypia and the remaining seven (17.5%) were normal.
On the other hand, all of the 35 (100%) patients who were diagnosed with benign breast lumps by histopathology were found to be normal by GFNAC (though, 5 (14.3%) revealed mild atypical changes), as shown in Table 1.
Table 1: Camparative of FNAC findings by histopathology results
| FNAC |
Histopathology |
| Breast Cancer (positive) |
Benign Tumors (negative) |
| n |
% |
n |
% |
| Direct FNAC |
Positive |
35 |
87.5 |
33 |
94.3 |
| |
Negative
|
5 |
12.5 |
2 |
5.7 |
|
Total |
40 |
100 |
35 |
100 |
| Grading FNAC |
Positive |
28 |
70 |
0 |
0 |
| |
Negative |
12 |
30 |
35 |
100 |
| |
Total |
40 |
100 |
35 |
100 |
These findings exposed Specificity of 94.3% and 100% in addition to sensitivity of 87.5%, 70% credited for CFNAC and GFNAC systems, respectively. In comparison of the FNAC results by the two examination systems (CFNAC and GFNAC); the two systems agreed in 27 (96.4%) specimens of the total 28 (100%) positive results by GFNAC. They similarly agreed in 37(96.4%) of the 38 (96.4%) negative diagnosis by FNAC.
Concerning the 35 benign conditions, 14 (40%) patients were ected with fibrocystic changes followed by fibroadenoma and ammatory changes constituting 8 (22.8%) and 5 (14.4%), pectively. Besides, there were 8 (22.8%) specimens found with mal tissue constituents. Most of these benign changes were ected among the younger patients unlike malignant changes, which mainly appeared to increase with an increase in age. (Table 2)
Table 2: Description of the study population by age and differential diagnosis of histopathology
| Pathology |
Age groups |
| <30 years |
31-40 |
41-50 |
51-60 |
61+ |
Total |
| Normal |
3 |
3 |
1 |
1 |
0 |
8 |
| Inflammatory |
5 |
0 |
0 |
0 |
0 |
5 |
| Fibroadenoma |
3 |
3 |
2 |
0 |
0 |
8 |
| Fibrocystic change |
2 |
4 |
5 |
2 |
1 |
14 |
| Malignant change |
4 |
11 |
12 |
10 |
3 |
40 |
| Total |
17 |
21 |
20 |
13 |
4 |
75 |
Discussion
Cancer continues to be the most feared disease that worries societies worldwide, and the current data ensures the increasing importance of the issue in the coming years. Despite the increasing technology in diagnostic medicine, the wide array of laboratory methods and sophisticated imaging techniques, biopsy interpretation is still the most vital, the most accurate and the most precise method on which the final diagnosis of cancer depends.
In the current study, and of a total of 75 patients with breast palpable lumps who visited a surgical unit at Khartoum Teaching Hospital; 40 (53.3%) were diagnosed with breast cancer and 35 (46.7%) were diagnosed with benign lesions. These variables clearly signify the risk of breast cancer in the Sudan. Nevertheless, the majority of patients with benign conditions were younger; hence, the great majority of the cancer patients were among the elder age groups. Moreover, most of these patients present with advanced stages of the disease. However, in the Sudan, as in most developing countries, there is a lack of screening programs (e.g. Mammography and other imaging system), as well as the absence of awareness towards cancer early detection (e.g. breast self examination). This is not the only explanation, but it is well-known that the risk of breast cancer increases with an increase in age, which was largely reported.11
This study deliberated the possibility of applying GFNAC in diagnosis of breast lesions, as compared to CFNAC in terms of specificity and sensitivity using histopathology.
The diagnostic accuracy of FNAC is defined as a correlation with histologic findings, depending on the availability of a good aspirate and good abilities of reporting. One of the major draw backs of this technique is to obtain an insufficient specimen. Therefore, a broad range of false positive rates (73% to 98%) were reported.4
CFNAC in the present study showed high Specificity (94.3%), and Sensitivity (87.5%), which were similar to the findings of many published works. Langmuir et al. (1989), reported an average sensitivity of 87%, specificity of 99% and positive predictive value of 97%.3 Another study compared a core biopsy using gun biopsy with FNAC and showed a sensitivity of 82% and specificity of 100%.12
With regard to the 5 (12.5%) cancer patients, who were found negative by CFNAC, unlike histopathology wherein tissue pattern, cell morphology, intracellular products and intracellular matrix are preserved, in cytology it is mainly cell morphology which is preserved.
The major disadvantage of FNAC is that some false negative diagnoses are inevitable. Since no test will be 100% accurate in most series, approximately 10% of the carcinomas cannot be diagnosed by FNAC.13 Similar results have been encountered (12.5%) in our series for CFNAC. The cytological findings of mucocele like tumor and mucinous carcinoma were found different in cellularity, shape of cell clusters and nuclear features, so these may indicate the possibility of reporting, such malignant neoplasms as benign, as occurred in our series.14 However, the same approaches were previously reported.15
Concerning the two cases that were reported as positive by CFNAC and proved to be negative by histopathology, false positive diagnosis of carcinoma may occur due to misinterpretation of atypical cytological changes. Poorly fixed aspirates and air-drying artifacts can be a potential source of error as cells are swollen and reveal nuclear atypia. The presence of large clusters of histiocytes with enlarged nuclei and degenerating apocrine cells mimic carcinoma.15
Though, GFNAC showed superior specificity but produced a low sensitivity, and as the assessment depend mostly on the nuclear features of malignancy, the high false negative findings 12 (30%) were expected. This system depends on certain criteria, which ignores some important feature for the diagnosis of breast cancer. In breast CFNAC, the cellularity of the smear, lack of cohesion between the cells and absence of myoepithelium are at least as important features of malignancy as the nuclear atypia itself. This in addition to the fact that the system is rather complicated and time consuming, though, the combined use of both systems may supports the accuracy of reporting. Therefore, these facts provide some sort of limitation to the applicability of this system in routine cytopathology reporting. However, GFNAC can be used to predict the degree of atypical changes in specimens diagnosed as suspicious of negative by CFNAC. Otherwise, the GFNAC might be more applicable in exfoliative cytology than in Aspiration cytology.
Conclusion
Overall, the results of this study suggest that, GFNAC system, with its employment restricted to exfoliative cytology, it cannot be a substitute for CFAC in the cytodiagnosis of breast lumps, though it has a high sensitivity; but due to its low sensitivity and complexity. Although, GFNAC is complicated and has low sensitivity, it supplements the accuracy of CFNAC and weight the benign breast lumps in term of cytological atypia.
Acknowledgements
We would like to thank to Fathia Eltyb at the Department of Histopathology and Cytology, Faculty of Medical Laboratory science, Alazhri University for her help and assistance. The author has no connection with any company and the work was supported by author and University of Khartoum.
|