Sister Mary Joseph nodules (SMJN) are malignant metastatic nodules involving the umbilicus. Metastasis most commonly originates from primaries in the gastrointestinal tract (GIT). GIT tumors, in order of frequency, include pancreatic carcinoma, gastric carcinoma, and colonic cancer. Primaries in the genitourinary tract (GUT) have been reported as SMJN.1 These cutaneous metastatic nodules are generally a sign of advanced malignant disease and carry poor prognosis.2 SMJN present as a painful lump on the anterior abdominal wall, with different morphological characters. Neuroendocrine tumors (NETs) are rare form of neoplasms, which are derived from peptide and amine hormone producing cells. They are subcategorized into carcinoid tumors, functional and non-functional NETs. Neuroendocrine tumors account for 0.5% of all malignancies.3
Case Report
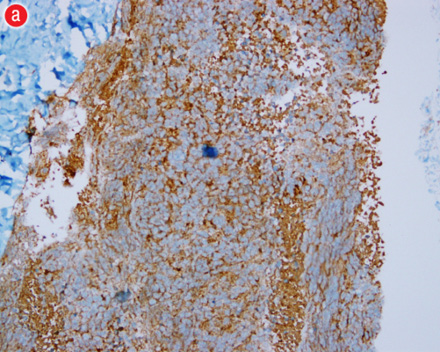
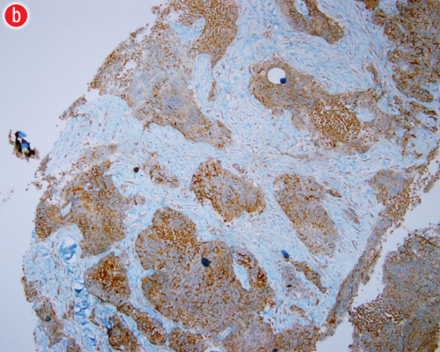
A 71-year-old man, with a history of diabetes mellitus and hypertension, was admitted to the King Fahad University Hospital complaining of painless umbilical swellings for several months. There was no history of constitutional, gastrointestinal or urinary symptoms and no fainting episodes, sweating or flushing. He denied any history of smoking or alcohol ingestion. On examination, the patient had normal vital signs. His abdomen was soft and lax with no tenderness. The liver was palpable 3cm below the costal margin but there was no splenomegaly. Local umbilical examination demonstrated a lobulated mass measuring 6cm by 8cm, which was firm and non-pulsatile without any signs of inflammation or ulceration. The skin was freely mobile over umbilical swelling and lobulated in nature [Figure 1]. The laboratory test showed white blood cells (WBC) 6.8k/µl, hemoglobin (Hgb) 9.5g/dL, and platelets 360k/µl. Bilirubin was within normal limits. Other measurements were, albumin 2.1g/dL, alkaline phosphatase 287IU/L, serum glutamic-oxaloacetic transaminase 65IU/L, serum glutamic pyruvic transaminase 39IU/L, lactate dehydrogenase (LDH) 429IU/L, and gamma-glutamyl transpeptidase 272IU/L. Carcinoembryonic antigen (CEA) was elevated 8.3ng/ml (normally <2.5ng/ml), carbohydrate antigen (CA) was 19-9<2U/ml and alpha-fetoprotein (AFP) was 1.61ng/ml. Erythrocyte sedimentation rate (ESR) 102mm/h was elevated and 24-hour urinary 5-hydroxyindoleacetic acid (5-HIAA) concentration was normal. Computed tomography (CT) of the abdomen showed para-umbilical mass [Figure 2] and multiple lesions in liver suggestive of metastasis [Figure 3]. A Tru-cut biopsy was performed and histopathological examination revealed mass tissues consistent of small groups of malignant pleomorphic cells with marked stromal dysplasia in between. Immunohistochemical studies showed positive immunoreactivity of neoplastic cells to cytokeratin and chromogranin [Figure 4a and b], and negative reactivity with AFP, CEA, vimentin, leukocyte common antigen (LCA), CD20 antigen, and neuron-specific enolase (NSE). The final histopathological diagnosis was consistent with a neuroendocrine tumor. Unfortunately, during the work up and staging, the patient had a cardiopulmonary arrest and died.

Figure 1: Umbilical swelling, lobulated in nature with some skin changes.

Figure 2: Computed tomography of the abdomen revealing the umbilical tumor (red arrow).

Figure 3: Computed tomography of the abdomen showing liver metastasis (red arrow).
|
|
|
|
|
|
Figure 4: (a) Chromogranin immuno-histochemistry staining in brown confirming neuroendocrine nature of the umbilical nodule with all features of the neuroendocrine origin. (b) Higher magnification of chromogranin staining in brown confirming the findings of neuroendocrine origin |
Discussion
SMJN are malignant metastasis involving the umbilicus accounting for 10% of all secondary tumors to the skin.1 The condition was named after Sister Mary Joseph (1856-1939) a religious nurse from the future Mayo clinic who first noticed the relationship between umbilical metastasis nodule with advanced inoperable malignancy. SMJN usually present as a painful lump on the anterior abdominal wall with different morphological characters, including ulceration, but in our patient it was not painful and non-tender. Metastasis to the umbilicus can occur in several ways. Contiguous spread of peritoneal cancer to the anterior surface of the abdominal cavity is probably the most common and hematogenous spread through the arterial and venous systems via communication between the umbilical veins, portal system and the caval vein system. Lymphatic spread via lymphatic channels that communicate with axillary, inguinal and periaortic lymph nodes is also possible. Direct extension along the ligaments of embryonic origin have been described including the round ligament of the liver, the urachus, the vittelointestinal duct remnant, and the obliterated vitelline artery.1 These ligaments communicate with the umbilicus and contain remnants of the obliterated fetal structures.4
Neuroendocrine tumors (NET) are tumors arising from neuroendocrine cells of neural crest origin. They are characterized by the presence of neurosecretory granules that react positively to silver stains and to specific markers including neuron specific enolase, synaptophysin and chromogranin. The most common NET are carcinoid tumors, which arise from enterochromaffin cells that are distributed throughout the GIT and secret serotonin. There are several genetic syndromes that increase the risk for their development such as Multiple Endocrine Neoplasia 1 and 2 (MEN1 and MEN2), and neurofibromatosis.5 Clinical presentation of these is variable. Patients with functional NET present with symptoms of over production of certain hormones. For example, carcinoid tumors present with symptoms of over production of serotonin that manifest with symptoms of flushing, diarrhea, asthma, and carcinoid heart disease, none of which our patient had indicating a non-functional type. Other patients may present with metastasis in up to 22% of the cases.6 Most commonly they metastasize to the liver, as seen in our patient. The combination of NET and SMJN has not been reported.
In men, the most common primary for SMJN is GIT tumors in which the gastric and pancreatic cancers are the most common in the group. In women, epithelial ovarian tumors are the most common primary sites.7 The role of surgical treatment is limited in these metastatic nodules as they indicate advanced disease with poor prognosis. Palliative chemotherapy is considered in such an advanced case, namely Fluorouracil (5-FU).8 Some reported the use of interferon-alfa and interferon-beta with varying degrees of survival improvement.9 With improved targeted therapy, some authors advocated surgical debulking and institution of multimodalities to control the disease. It is difficult to validate such an approach due to the rarity of the disease.
Conclusion
In conclusion, SMJN is a rare entity and even rarer is NET as a cause. Umbilical swellings have many etiologies depending on age and whether it is malignant or benign in nature. SMJ nodule occurs commonly as a result of underlying pancreatic malignancy. A neuroendocrine tumour should be suspected as a possible cause as demonstrated by this case.
Disclosure
The author declared no conflict of interest. No funding was received for this work.
Acknowledgements
We would like to thank Professor Maha Abdulahadi, consultant of general surgery, for her guidance in the management of this case.
references
- António Murinello, Ana Carvalho, João Freire, A. Manuel Figueiredo, Marta Baptista, Helena Damásio, et al. Sister Mary Joseph’s nodule. GE - J Port Gastrenterol 2010;17:266-270.
- Abdulqawi R, Ahmad S, Ashawesh K. A rare cause of Sister Mary Joseph’s nodule. Swiss Med Wkly 2007 Oct;137(39-40):559-560.
- Taal BG, Visser O. Epidemiology of neuroendocrine tumours. Neuroendocrinology 2004;80(Suppl 1):3-7.
- Powell FC, Cooper AJ, Massa MC, Goellner JR, Su WP. Sister Mary Joseph’s nodule: a clinical and histologic study. J Am Acad Dermatol 1984 Apr;10(4):610-615.
- Calender A. Molecular genetics of neuroendocrine tumors. Digestion 2000;62(Suppl 1):3-18.
- Seemann MD, Meisetschlaeger G, Gaa J, Rummeny EJ. Assessment of the extent of metastases of gastrointestinal carcinoid tumors using whole-body PET, CT, MRI, PET/CT and PET/MRI. Eur J Med Res 2006 Feb;11(2):58-65.
- Abdulqawi R, Ahmad S, Ashawesh K. A rare cause of Sister Mary Joseph’s nodule. Swiss Med Wkly 2007 Oct;137(39-40):559-560.
- McCollum AD, Kulke MH, Ryan DP, Clark JW, Shulman LN, Mayer RJ, et al. Lack of efficacy of streptozocin and doxorubicin in patients with advanced pancreatic endocrine tumors. Am J Clin Oncol 2004 Oct;27(5):485-488.
- Pavel ME, Baum U, Hahn EG, Schuppan D, Lohmann T. Efficacy and tolerability of pegylated IFN-alpha in patients with neuroendocrine gastroenteropancreatic carcinomas. J Interferon Cytokine Res 2006 Jan;26(1):8-13.