|
Abstract
Objective: This study aimed to evaluate the mortality pattern in children seen at Federal Medical Centre Umuahia (FMCU) Abia state, South Eastern Nigeria.
Methods: A retrospective cross sectional descriptive study over a 5-year period from January 1, 2004 to December 31, 2008 using data retrieved from the hospital’s medical records department.
Results: A total of 3,814 children were admitted in the hospital and 434 of them died giving a mortality rate of 11%. The mean age was 1.7 (Std D of 3.19). Two hundred and thirty eight of them were males while 196 of them were females giving a sex ratio of 1.2:1. Majority of the mortality (49%) occurred within 24 hours of admission. The major causes of death during neonatal period were birth asphyxia (34%), prematurity (24%) and neonatal sepsis (24%). Malaria was the leading cause of death beyond the neonatal period accounting for 42% of cases. Other common mortality causes were pneumonia, septicaemia, diarrhea, HIV AIDS and meningitis each accounting for 10%, 10%, 7%, 7% and 5% respectively. The months of July, May and March accounted for most deaths (12%, 12% and 11% respectively).
Conclusion: Birth asphyxia and malaria associated deaths were responsible for most deaths during neonatal and beyond neonatal periods respectively. Presence of trained personal at all deliveries will help to reduce neonatal asphyxia. Efforts should be made to reinforce the existing effective malaria control tools.
Keywords: Mortality pattern; Causes of death; Childhood; Admission duration.
Introduction
The WHO convention on the rights of the child, defines a child as a person below the age of 18 years, unless the laws of a particular country set the legal age for adulthood younger.1,2 Childhood age group are a special group of people that need special care and protection that adults do not.1,2 In the year 2010, 7.6 million children died all over the world before reaching the age of 5 years. Of this large number, 64% were attributable to infectious diseases with pneumonia, diarrhea and malaria topping the list.3,4 Most of these deaths (more than 80%) occur in poor countries in sub-Saharan Africa and South Asia including India, Nigeria, Democratic Republic of the Congo, Pakistan and China.4-7 Reports on the ‘state of the world’s children’ indicate an overall decline in child mortality from 100/1000 children in 1999 to 72/1000 children in 2010. Some countries even achieved 50% reduction between 1990 and 2010 (countries in North America, Eastern Europe, South east Asia and in Latin America).3
In South America, the major cause of childhood mortality were due to respiratory infections.8 Various studies in different parts of Africa reported malaria as the highest cause of childhood deaths.9,10 Studies from different Nigerian centers had infectious disease as the commonest cause of death but reported different types of infections ranging from HIV AIDS, to septicaemia to malaria, malnutrition and diarrhea diseases.11-14 The development and evaluation of effective programs to reduce the burden of disease requires a detailed knowledge of disease or mortality distribution and causal pathways.15 Child survival efforts can be effective only if they are based on accurate information about causes of deaths.16 This study is, therefore, aimed at evaluating the mortality pattern in children seen at Federal Medical Centre Umuahia (FMCU), with a view to evaluating services and identifying areas for improved care. FMCU is located in the metropolis of Umuahia, the capital of Abia state, South-eastern Nigeria with most of the populace being low income earning traders and few civil servants (government employees). There is only one government owned primary health center in the town and is not functioning optimally, thus our hospital serves both as a general and referral health facility. Majority of children seen in our center were coming as their first contact with a health facility following their sickness. Patients in the area normally come to the hospital as first health facility since it is the only fully functional public hospital with enough doctors and specialists in various fields of medicine. Few are referred from private owned hospitals because they lack a specialist (pediatrician) and special equipments that may be needed in to manage difficult cases. There are no previous available data on childhood mortality from our hospital or the health facilities in the State.
Methods
This was a retrospective cross sectional descriptive study over a 5 year period from January 1, 2004 to December 31, 2008. Data, for the study, was retrieved from the hospital’s medical records department. Records of children aging from birth to 14 years of age, who died in the hospital, were reviewed. Data extracted from the records included age, sex, principal diagnosis/cause of death and duration of hospitalization before death. Post mortem examination was not done for the patients because of lack of facility and manpower for this service. The diagnosis and cause of death were largely clinically based with supportive laboratory results. Data collected was entered into a spread sheet using SPSS software package version 16.0. Descriptive statistics was used to analyze the obtained data and a p-value of ≤ 0.050 was considered significant.
Results
During the 5 years study period, a total of 3,814 children were admitted in the hospital and 434 of them died giving a mortality rate of 11%. The mean age was 1.7 (Std D of 3.19) with minimum and maximum ages of a day old and 15 years respectively. Two hundred and thirty eight of them were males while 196 of them were females giving a sex ratio of 1.2:1. Neonates accounted for 40% of cases, while infants (2-12 months), age group 1-4 years, age group 5-9 years and age group 10-15 years each accounted for 25%, 22%, 7% and 6% respectively as shown in table 1. Table 2 shows the duration of stay on admission before mortality. Majority of the mortality (49%) occurred within 24 hours of admission. Thirty eight percent occurred between 2-6 days on admission with 51% of them occurring after 48 hours of admission and 16% of them occurring after 72 hours of admission (p=0.050).
Table 1: Age and sex distribution of cases.
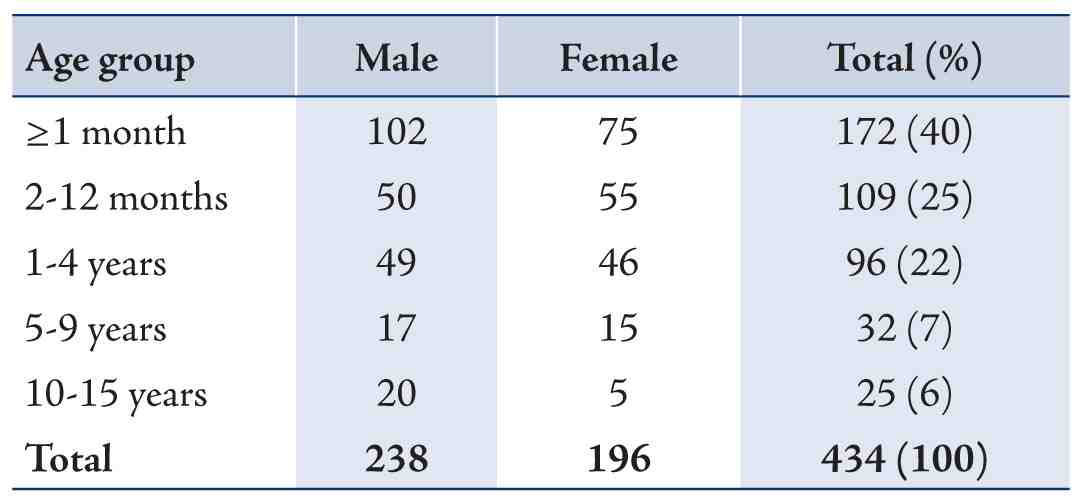
Table 2: Duration of hospitalization before death.

Table 3 shows the various causes of death in neonates. The major diseases in neonatal period were birth asphyxia (34%), prematurity (24%) and neonatal sepsis (24%). Other causes were neonatal jaundice (8%) and low birth weight (6%). Table 4 shows the various diseases causing deaths in children in post neonatal period. Malaria was the leading cause of death accounting for 42% of cases. Other common mortality causes were pneumonia, septicaemia, diarrhea, HIV AIDS and meningitis each accounting for 10%, 10%, 7%, 7% and 5% respectively.
Figure 1 shows the monthly pattern of mortality. The months of July, May and March accounted for most deaths (12%, 12% and 11% respectively). Other months with high mortality were September (10%), January (9%) and June (8%).
Table 3: Causes of neonatal deaths.
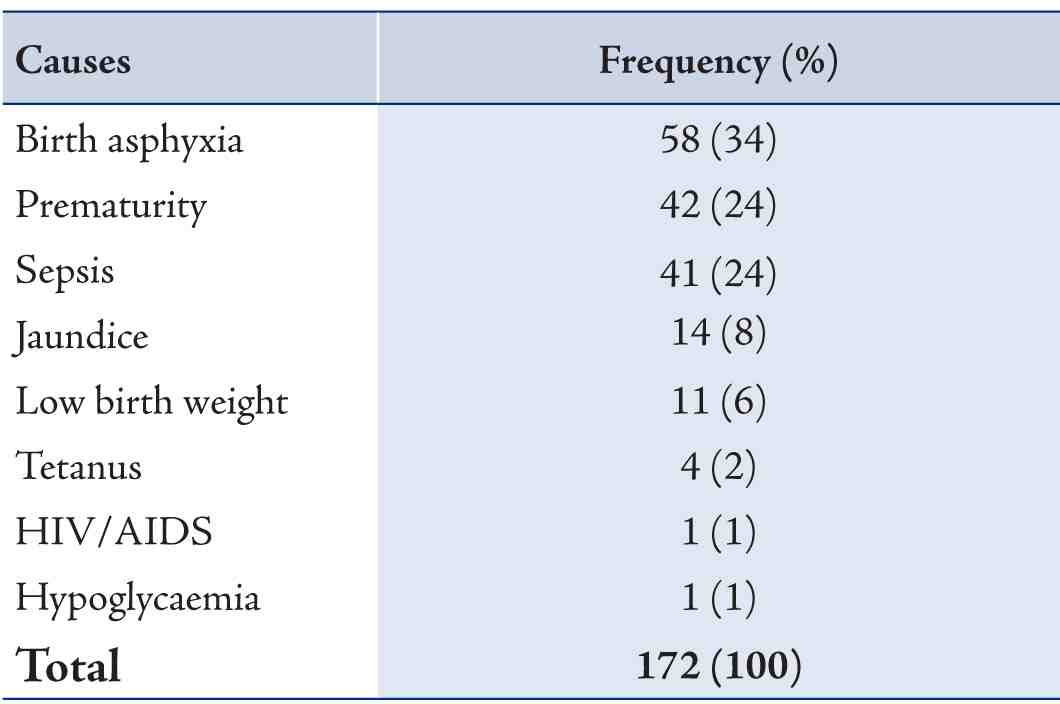
Table 4: Causes of death after neonatal period.
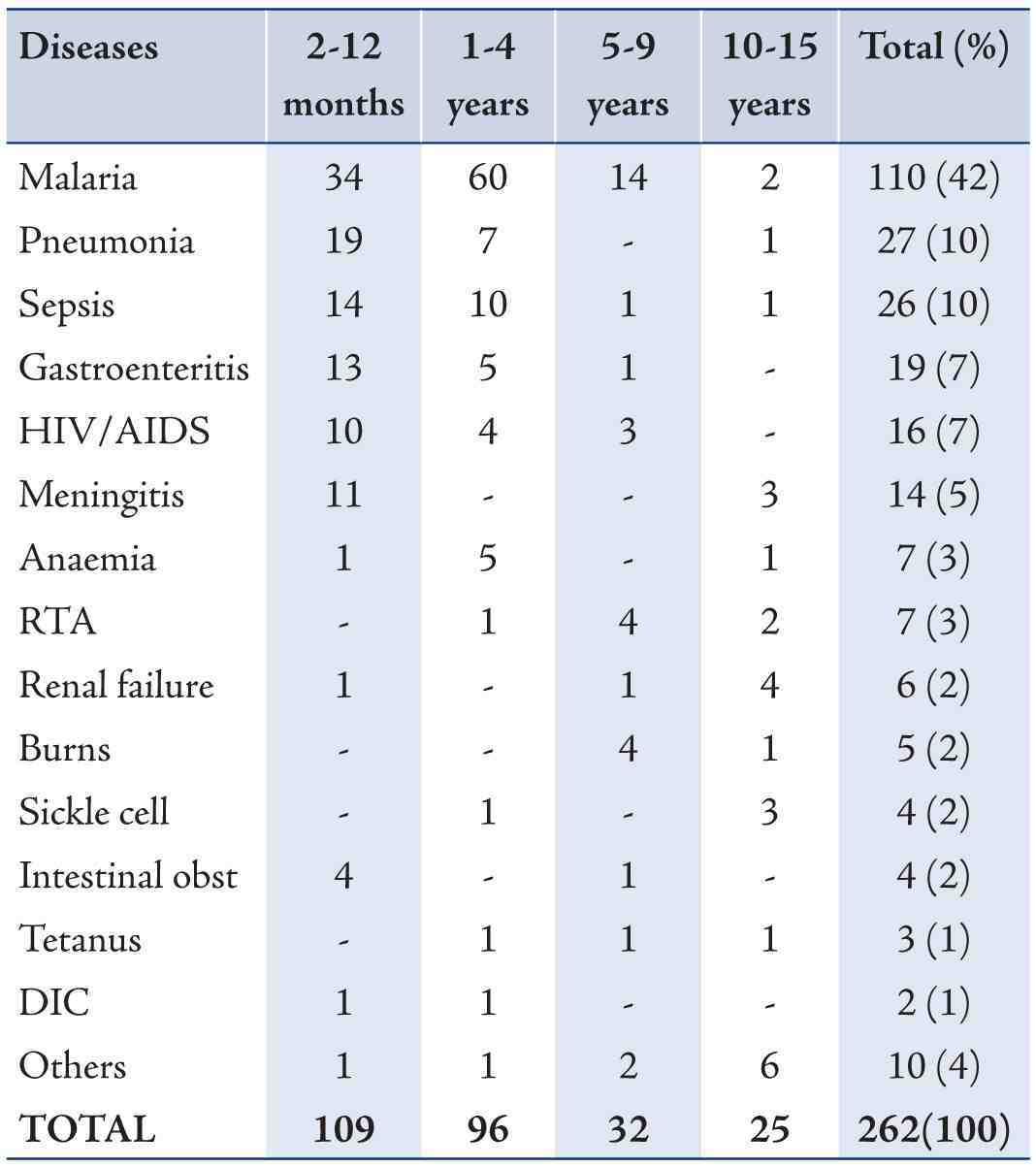
RTA= Road traffic accident, DIC= Disseminated intravascular coagulation, Obst= Obstruction.
Others include all diseases that caused death in only one person and include the following; rheumatic heart disease, hepatitis, typhoid perforation, epilepsy, leukaemia, malnutrition, hydrocephalus, ewings sarcoma, gunshot and electrocution.
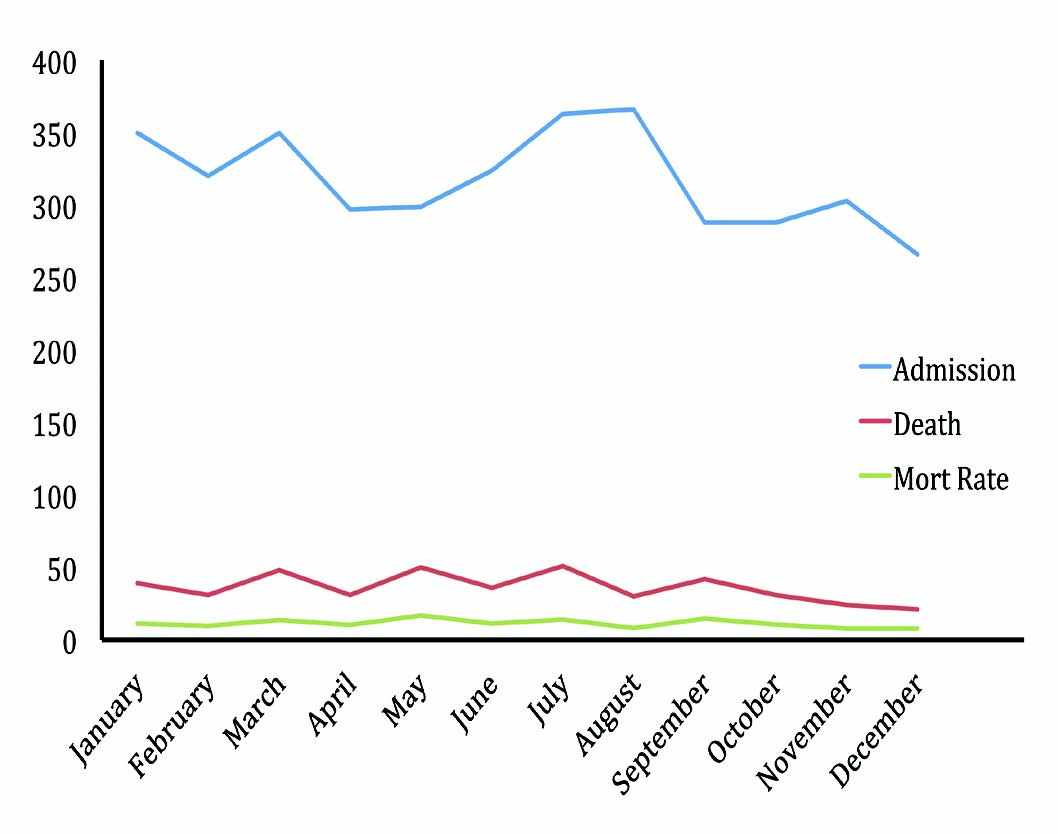
Figure 1: Monthly pattern of mortality.
Discussion
Childhood mortality is a major public health problem in Sub-Saharan Africa and for the implementation of efficient public health systems, knowledge of the spatial distribution of mortality is required.15 Observations from hospital based mortality data have major limitations including the following; incomplete reporting of deaths seen more in developing countries, lack of accuracy (that is inaccuracies in recording age and cause of death. The cause of death is often inaccurate or incomplete due to difficulties such as lack of diagnostic evidence, inexperience on the part of the certifying doctor and absence of postmortem which may be important in deciding the cause of death).17 Most deaths in Nigeria are not registered; therefore, it is not possible to generate comprehensive population-based mortality data hence hospital-based data recorded by medically-qualified staff are used and can yield useful information to characterize mortality which has occurred.18 In Nigeria, the need to reduce childhood morbidity and mortality is one of the greatest health challenges confronting the federal government.19 Despite the efforts of successive governments to tackle the problem, the results have been dismally poor.19 The mortality rate in this study was 11%. This is similar to 11% and 12% reported in some other parts of the country.11,20 Though this rate is lower than 15% reported in Zaria (Nigeria) and higher than 8% reported in both Kenya and South Africa (African Countries).21-23
Neonatal deaths accounted for most of childhood deaths (40%) in this study, followed by infant deaths (25%). This is similar to findings in Lagos and Shagamu where neonatal deaths accounted for most childhood deaths though our rate is less.13,20 Globally 40% of deaths in children younger than 5 years occurred in the neonatal period, most often because of preterm birth complications, intrapartum related complications and neonatal sepsis or meningitis, with India, Nigeria, Democratic Republic of the Congo and Pakistan accounting for 53% of neonatal deaths.7 Three leading causes of neonatal deaths in this study were birth asphyxia (34%), prematurity (24%) and neonatal sepsis (24%).This is similar to findings in Lagos, Ibadan, Ilorin and Oman.13,24-26 Perinatal mortality is a useful measure of the socio-economic status of a community and a standard of obstetric care provided within the community.27 Studies have shown that medical attention at the time of delivery and antenatal care are significant factors in the survival chance of a new born.13,28 The high rate of birth asphyxia recorded, calls for intensification of programs like “Neonatal resuscitation” and “Helping babies breathe”.13 The high rate of asphyxia may be due to lack of access to and poor utilization of available health care services and is a pointer to the need for more health care providers to be trained in neonatal resuscitation especially at the community level.13 Beyond the neonatal period, the major causes of childhood deaths were severe malaria (42%), pneumonia (10%), septicaemia (10%), diarrhea (7%) and HIV AIDS (7%). These major causes are similar to findings from previous Nigerian and African studies, though their individual rates varies.9-11,13,14,20,22
Malaria as the highest cause of childhood mortality as seen in this study was also reported in Abakiliki (Nigeria), Eldoret (Kenya) and Upper River Division (Gambia).9-11 The high burden of malaria deaths in our environment may be due to high levels of parasite resistance to affordable drugs, high cost of artemesinin based combination drugs and inadequate provision/scarcity of insecticide treated nets.11 Apart from the above mentioned reasons, late presentation to hospital for treatment also plays a major role and this cannot clearly be separated from educational and economic powers of the parents.11,13 Interventions like roll back malaria need to be intensified.11
Pneumonia is the highest cause of non-neonatal under 5 mortality (14%) globally.7 Pneumonia accounted for 10% of mortality in the index study. This is similar to findings in Lagos, Jos and less findings in Port Harcourt, Kenya, Harare and Abakiliki.11-14,22,29 Common to most studies, was that most of the victims of pneumonia were infants, like in the index study. The high prevalence of pneumonia in infants may be due to increased susceptibility to infections due to a combination of immature host immune system and constant contact with numerous viral and bacterial agents in the environment.30 Health education about reduction of risk factors for pneumonia (especially overcrowding) and improved housing condition will help to reduce its prevalence. Diarrhea diseases accounted for 7% of cases. This is higher than 5%, 6% and 6% reported in Lagos, Port Harcourt and Eldoret Kenya but much lower than 16% and 23% reported in Jos and Abakiliki respectively.11-14,22 Mortality from diarrhea can be reduced further by increasing awareness and use of oral rehydration solution by most mothers, improved sanitation and appropriate feeding practices.
HIV/AIDS accounted for 7% of mortality. This is higher than 5% reported in Lagos and less than 21% reported in Port Harcourt.13,14 Globally HIV/AIDS caused 2% of childhood deaths.7 Child mortality estimates from community based cohorts demonstrate that the children of HIV infected mothers have higher mortality rates than the children of uninfected mothers and that child mortality is closely linked with maternal health status.31 Efforts should be made such that all infected mothers are counseled and treated so as to reduce vertical transmission to children through effective prevention of mother to child transmission (PMTCT) and Early Infant Diagnosis (EID).
Forty-nine percent of childhood deaths in the index study occurred within less than 24 hours of admission, while 26% of deaths occurred after 2-3 days on admission. This finding is similar to 49% reported in Jos and higher than 25%, 40% and 44% reported in Abakiliki, Zaria and Zimbabwe respectively.11,12,21 However, studies in Lagos and Kenya reported higher rates of 55% and 65%.13,22 One common denominator in all these high mortality within 24 hours is late presentation to hospitals by parents with their children.12,21 Most times before this late presentation, self medication, visit to chemist or traditional healers or prayer homes have taken place and the scarce resources already spent. On few occasions when they present early, insufficient funds may also delay the purchase of prescribed drugs which may increase mortality. Health education, provision of affordable, accessible health care and functional well spread out health insurance scheme will help to increase early utilization of health facilities. This is necessary because income inequality and cultural beliefs prevent people from taking full advantage of existing health facilities.32,33 Also issues like education, female autonomy, women’s work status and economic condition of the household are known to influence child mortality.34
Seasonal variation in mortality is a well known fact.35 Mortality ranged from 21% - 51% with the high rates occurring most in rainy months and lowest of 24% and 21% occurring in November and December respectively. This is similar with reports from Abakiliki, Jos, Port Harcourt, Burkina Faso and Gambia.9-12,14 Increased mortality during the raining/wet season may be explained by our finding that the major causes of deaths such as malaria, pneumonia and diarrhea diseases occurred more frequently during the raining season. This is because mosquitoes breed better during wet season and wet seasons also provides chilling environment for micro organisms that cause pneumonia and contamination of sources of drinking water.11,13,14 The major limitations of the index study are that it was a retrospective study and autopsy was not done on any of the cases. Without an autopsy the cause of death can be wrong in as many as 30% of cases, although autopsies do not always provide the cause of death.36
Conclusion
The pattern of childhood mortality in Umuahia has been documented. The results from this study confirm that high neonatal deaths were mainly due to birth asphyxia while after neonatal period, mortality due to malaria infection ranked highest. Since neonatal asphyxia and malaria were seen to be the major causes of childhood mortality, efforts to reinforce the existing malaria control tools and attempts at reducing birth asphyxia should be implemented.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. Unicef Fact Sheet. A summary of the rights under the convention on the rights of the child. Available at: [cited and updated: 3rd October, 2013] http:// www. Unicef. Org /crc/ files/ rights overview pdf.
2. Unicef. The state of the world’s children 2012. Convention on the rights of the child 2012. Available at: [cited and updated: 3rd October, 2013] http:// www. Unicef .org/crc.
3. Unicef. The state of the world’s children, 2010. Unicef Annual Report.
4. The inter-agency group for child mortality estimation (IGME). Estimates of under five mortality rates by country, the 2011 release. Available at: [cited and updated: 3rd October, 2013] http:// www. Child mortality. org.
5. Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet 2003 Jun;361(9376):2226-2234.
6. Cabral SA, Soares de Moura AT. Overview of the global health issues facing children. Pediatric 2012; 129 (1): Dol: 10. 1542/ peds. 2011-2665.
7. Liu L, Johnson HL, Perin J, Scott S. Lawn JE etal. Global, regional and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 2012 .
8. Victora CG, Barros FC, Huttly SR, Teixeira AM, Vaughan JP. Early childhood mortality in a Brazilian cohort: the roles of birthweight and socioeconomic status. Int J Epidemiol 1992 Oct;21(5):911-915.
9. Hammer GP, Somé F, Müller O, Kynast-Wolf G, Kouyaté B, Becher H. Pattern of cause-specific childhood mortality in a malaria endemic area of Burkina Faso. Malar J 2006;5:47.
10. Jaffar S, Leach A, Greenwood AM, Jepson A, Muller O, Ota MO, et al. Changes in the pattern of infant and childhood mortality in upper river division, The Gambia, from 1989 to 1993. Trop Med Int Health 1997 Jan;2(1):28-37.
11. Mouneke UV, Ibekwe RC, Eke CB, Ibekwe MU, Chinawa JM. Mortality among paediatric inpatients in mile 4 mission hospital Abakiliki, South-eastern Nigeria: a retrospective study. Niger J Paediatr 2013;40(3):259-263.
12. Ighogboja IS, Angyo I, Okolo AA, Szlacheka R. Morbidity and mortality patterns of paediatric emergencies in Jos Nigeria. Niger Med Pract 1995;30(1/2):15-18.
13. Fajolu IB, Egri-okwaji MT. Childhood mortality in children emergency centre of the Lagos University Teaching Hospital. Niger J Paediatr 2011;38(3):131-135 .
14. George IO, Alex-Hart BA, Frank-Briggs AI. Mortality pattern in children: a hospital based study in Nigeria. Int J Biomed Sci 2009 Dec;5(4):369-372.
15. Sankoh OA, Yé Y, Sauerborn R, Müller O, Becher H. Clustering of childhood mortality in rural Burkina Faso. Int J Epidemiol 2001 Jun;30(3):485-492.
16. Bryce J, Boschi-Pinto C, Shibuya K, Black RE; WHO Child Health Epidemiology Reference Group. WHO estimates of the causes of death in children. Lancet 2005 Mar;365(9465):1147-1152.
17. Park K. Principles of epidemiology and epidemiologic methods. In Park K (ed): Park’s textbook of preventive and social medicine. 22nd Ed. Banarsidas Bhanhot, Jabalpur India 2013, pp 50-77.
18. Preacely N, Biya O, Gidado S, Ayanleke H, Kida M, Akhimien M, et al. Hospital-based mortality in Federal capital territory hospitals-Nigeria, 2005-2008. Pan Afr Med J 2012;11:66-71.
19. Asakitikpi AE. Born to die: The ogbanje phenomenon and its implication on childhood mortality in southern Nigeria. Anthropologist 2008;10(1):59-67.
20. Fetuga B, Ogunlesi T, Adekanbi F, Olanrewaju D, Olowu A. Comparative analysis of childhood deaths in Sagamu, Nigeria: Implications for the fourth MDG. SAJCH 2007;1:106-111.
21. Wemmanda RD, Alli FU. Conditions associated with risk of death within 24 hours of admission in Zaria, Nigeria. Ann Afr Med 2004;3:134-137.
22. Menge I, Esamai F, van Reken D, Anabwani G. Paediatric morbidity and mortality at the Eldoret district hospital Kenya. East Afr Med J 1995 Mar;72(3):165-169.
23. Krug A, Patrick M, Pattinson RC, Stephen C. Childhood death auditing to improve paediatric care. Acta Paediatr 2006 Nov;95(11):1467-1473.
24. Adeyokunmu AA, Taiwo O, Antia AU. Childhood mortality among 22255 consecutive admissions in the University College Hospital Ibadan. Niger J Paediatr 1980;7:7-15.
25. Fagbule D, Joiner JT. Pattern of childhood mortality at University of Ilorin Teaching Hospital. Niger J Paediatr 1987;14:1-5.
26. Abdellatif M, Ahmed M, Bataclan MF, Khan AA, Al Battashi A, Al Maniri A. The patterns and causes of neonatal mortality at a tertiary hospital in oman. Oman Med J 2013 Nov;28(6):422-426.
27. Wilkinson D. Perinatal mortality-an intervention study. S Afr Med J 1991 May 4;79(9):552-553.
28. Zacharia KC, Irudayararajan S, Sarma K, Navaneetham PS, Nair G et al. Demographic transition in Kerala in the 1980s. Triuandrum: centre for development studies 1994.
29. Chawla V, Haufton B. Pattern of childhood mortality at Harare Central Hospital, Zimbabwe. East Afr Med J 1988 Apr;65(4):238-245.
30. Eigner FD. Cough and fever in children. Trop Doct 1981 Jan;11(1):31.
31. Newell ML, Brahmbhatt H, Ghys PD. Child mortality and HIV infection in Africa: a review. AIDS 2004 Jun;18(Suppl 2):S27-S34.
32. Ghosh R. Child mortality in India: a complex situation. World J Pediatr 2012 Feb;8(1):11-18.
33. Mondal NI, Hossain K, Ali K. Factor’s influencing infant and child mortality: A case study of Rajshahi district, Bangladesh. J Hum Ecol 2009;26(1):31-39.
34. Basu AM, Stephenson R. Low levels of maternal education and the proximate determinants of childhood mortality: a little learning is not a dangerous thing. Soc Sci Med 2005 May;60(9):2011-2023.
35. McKee M, Sanderson C, Chenet L, Vassin S, Shkolnikov V. Seasonal variation in mortality in Moscow. J Public Health Med 1998 Sep;20(3):268-274.
36. Burton JL. The history of the autopsy. In Burton JL and Rutty GN(eds): The Hospital Autopsy. 3rd Ed. Hodder Arnold London 2010, pp 1 - 10.
|