|
Abstract
Xeroderma pigmentosum is an uncommon inherited autosomal recessive disorder. Affected patients have a 2000-fold amplified risk of skin cancer. There is an inability to repair the damage to genetic material caused by ultraviolet light. Basal cell carcinoma is the most commonly associated carcinoma followed by squamous cell carcinoma and melanoma. It is a highly mutilating disorder where occurrence of multiple cancers and repeated surgical treatments result in serious psycho-social implications. We present a case of diagnosed xeroderma pigmentosum in a 25 year old male who presented with multiple lesions and non-healing ulcers on face. Four surgical specimens from left lower eyelid, chin, right cheek and upper lip were taken for histopathological diagnosis. Microscopic examination revealed five different tumors from biopsies of these sites - specimen from right cheek revealed two morphologically distinct tumors. The tumors include basosquamous carcinoma, nodular basal cell carcinoma, adenoid basal cell carcinoma, malignant melanoma and cavernous hemangioma.
Keywords: Xeroderma pigmentosum; squamous cell carcinoma; basal cell carcinoma; malignant melanoma; cavernous hemangioma.
Introduction
Xeroderma pigmentosum (XP) is an unusual, inherited autosomal recessive disorder which is characterized by increased susceptibility of skin cancer due to defective repair of Ultraviolet (UV) light-induced damage to genetic material.1-3 Hypersensitivity to solar irradiation is seen in this rare hereditary syndrome due to defect in nucleotide excision repair; and predisposition to basal and squamous cell carcinomas as well as malignant melanomas appearing at an early age has been well established.4
Case Report
We report a case of diagnosed xeroderma pigmentosum in a male of 25 years who presented with multiple lesions and non-healing ulcers on the facial area in May 2010. Five morphologically distinct simultaneous tumors were revealed during the microscopic examination of these lesions.
Tracing the patient history; there was nothing wrong at birth. At the age of 1 year, parents noticed that the child was unable to perceive the surroundings and respond accordingly. Loss of eyelashes was also noticed. The child was evaluated by a number of ophthalmologists and a markedly decreased vision was established along with corneal opacification and mild keratitis. However, there was no improvement in the symptoms despite treatment and the cause of this decreased vision remained unidentified.
One year later i.e. at the age of 2 years, tanning of skin and multiple dark spots were observed all over the body of the child. Six years later at the age of 8, the child had a surgical biopsy from skin lesions at left lip and cheek; it was reported as basal cell carcinoma on histopathology. Based on clinical examination and a strongly suggestive relevant history, the child was diagnosed as having xeroderma pigmentosum; however, tests for cellular hypersensitivity to UV damage and detection of defect in nucleotide excision repair were not done as they are time consuming, expensive and highly specialized.
Clinical record available with the patient showed that he underwent surgery at 12, 13, 22 & 23 years of age on different sites including forehead, head, nose, lower eyelid, cheek and lower lip. The biopsies showed squamous cell carcinoma, basal cell carcinoma and hemangioma at different times. Nonetheless, the patient never had any neurological complaint nor did the available clinical record showed any such abnormality.
Now at the age of 25 years, patient presented with photophobia and multiple lesions and non-healing ulcers again which were surgically excised. When examined light perception was intact but vision was severely impaired. Skin was dry parchment-like with obvious freckling. No neurological findings were observed.
Four surgical specimens from left lower eyelid, chin, right cheek and upper lip were taken during a single surgery on the face and evaluated for tissue diagnosis. The details are as under:
Lesion 1 (close to lower lid): Basosquamous carcinoma
The specimen measured 1.5x1.0 cm and its histological examination revealed tumor cells with abundant cytoplasm and more marked keratanization as compared to typical BCC and there were distinct areas of squamous differentiation. (Fig.1.) Palisading was focally lost at places. Ulceration was present and all the limits were involved by the tumor.
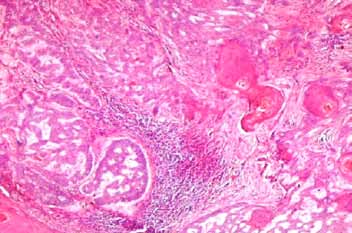
Figure 1: Basosquamous BCC.
Lesion 2 (on chin): Nodular Basal Cell Carcinoma
The specimen, measuring 1.5x1.0 cm, revealed typical large lobules and bands of basaloid cells associated with scanty cytoplasm and peculiar peripheral palisading nuclei. Artefactual retraction was also present. (Fig.2). All the limits were involved by the tumor.
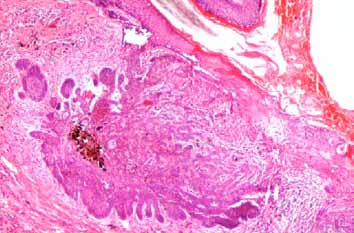
Figure 2: Nodular BCC.
Lesion 3 (on right cheek): Adenoid Basal Cell carcinoma and Malignant Melanoma
Surprisingly, this specimen that measured 1.8x 1.2 cm revealed two distinct tumors. In one area, there were thin strands of basaloid cells in a reticulate pattern alongwith stromal mucin (Fig.3) while another area showed atypical melanocytes having large nuclei and nucleoli with abundant pale cytoplasm spreading in a pagetoid fashion throughout the epidermis (Fig.4). The distribution of melanocytes and melanin pigment was highly irregular.
Lesion 4 (on upper lip): Cavernous Hemangioma
The specimen, measuring 2.0x1.8cm, showed poorly circumscribed collections of large ecstatic vessels (Fig.5). The vessels have thicker walls and occasionally contain intraluminal thrombi.
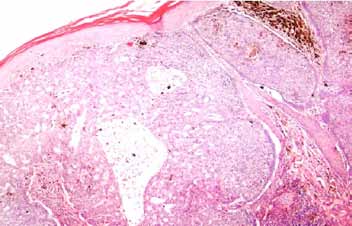
Figure 3: Adenoid BCC.
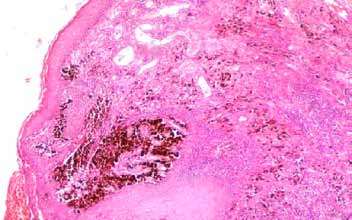
Figure 4: Malignant Melanoma.
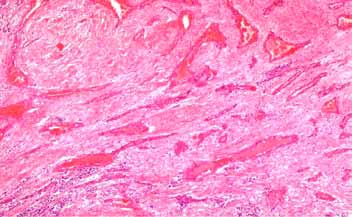
Figure 5: Cavernous Hemangioma.
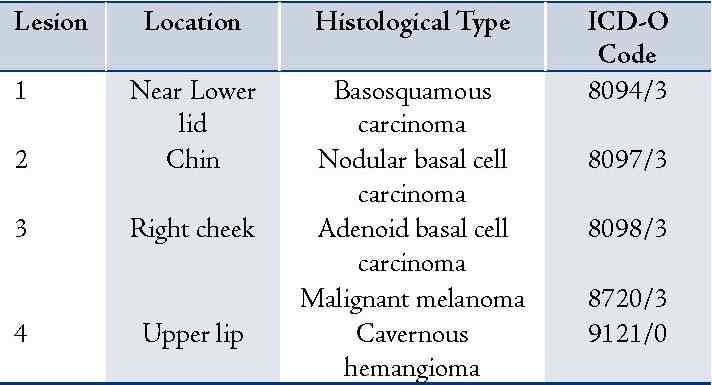
Table 1: Summary of location and five histological types of tumors with ICD-O codes, revealed from four lesions on face of an XP patient at one point in time.
Discussion
Xeroderma pigmentosum, first described by Hebra and Kaposi in 1874, is a rare genodermatosis whose occurrence is favored by consanguinity. Its frequency shows large geographical variations.4 XP occurs round the globe and has a prevalence of about 1:1,000,000 in the U.S and Europe.5 In countries with high levels of consanguinity, including Japan,6 North Africa and the Middle East, it is more common. In our case, parents of the patient were first cousins establishing consanguinity; nevertheless, all other siblings were normal. Pakistan has no centralized health records for incidence of XP, but there has been one published report of 36 cases of XP from Larkana, Pakistan estimating an average frequency of XP in the southern region of Pakistan to be about 1:100,000.7
The disease is associated with photophobia, cataract and other ocular lesions;4 similar features of corneal opacification, ciliary madarosis and decreased vision were present at the age of 1 year in this patient. Dry parchment-like prematurely aged skin, abnormal pigmentation and precocious cutaneous lesions are present in XP,4 and our patient has identical findings since the age of 2 years. Twenty percent of severely affected XP patients present neurological disorders of mental retardation as well as spasticity and microcephaly4 but our patient had no neurological sign or symptom. Similarly, none of the 36 cases of XP reported in Larkana, Pakistan had any neural changes.7
The main hallmarks of the cancer-prone, nucleotide excision repair deficient XP patients are hypersensitive to sunlight and a striking >2000-fold incidence of skin tumors.8 Multiple skin cancers arise at the median age of eight years in XP,4 to our wonder BCC was revealed from the first surgical biopsy taken from the cheek of the patient when he was 8 years old. This shows a dramatic contrast of a 50 year reduction in mean age of occurrence of Non-melanoma skin cancer in XP as compared to the general population.4
Basal cell carcinoma is the most commonly associated carcinoma followed by Squamous cell carcinoma and Melanoma,9 and in this patient we found two distinct types of BCC namely nodular basal cell carcinoma and adenoid basal cell carcinoma. The less commonly seen tumors in XP are keratoacanthomas, angiomas, fibromas and sarcomas,10 and an infected hemangioma was also present in this patient. A single lesion from right cheek revealed 2 tumors namely adenoid basal cell carcinoma and superficial spreading melanoma; such an incident has not been reported in literature before. Lastly basosquamous carcinoma from a lesion near lower lid was also present, simultaneously.
Conclusions
Three different types of tumors simultaneously in one patient have been reported by different studies worldwide.11-14 But here, to the best of our knowledge, we report the first case where five distinct histological forms of tumors were identified simultaneously on the face of a single patient.
Acknowledgments
The authors reported no conflict of interests and no funding was received for this work.
References
1. Kraemer KH, Patronas NJ, Schiffmann R, Brooks BP, Tamura D, DiGiovanna JJ. Xeroderma pigmentosum, trichothiodystrophy and Cockayne syndrome: a complex genotype-phenotype relationship. Neuroscience 2007 Apr;145(4):1388-1396.
2. Kraemer KH, Ruenger TM. Genome instability, DNA repair and cancer. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick’s Dermatology in General Medicine. Vol 7 ed. New York: McGraw Hill 2008; 977-86.
3. Ruenger TM, DiGiovanna JJ, Kraemer KH. Hereditary Diseases of genome instability and DNA repair. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick’s Dermatology in General Medicine. Vol 7 ed. New York: McGraw Hill 2008; 1311-25.
4. Daya-Grosjean L, Sarasin A. The role of UV induced lesions in skin carcinogenesis: an overview of oncogene and tumor suppressor gene modifications in xeroderma pigmentosum skin tumors. Mutat Res 2005 Apr;571(1-2):43-56.
5. Kleijer WJ, Laugel V, Berneburg M, Nardo T, Fawcett H, Gratchev A, et al. Incidence of DNA repair deficiency disorders in western Europe: Xeroderma pigmentosum, Cockayne syndrome and trichothiodystrophy. DNA Repair (Amst) 2008 May;7(5):744-750.
6. Hirai Y, Kodama Y, Moriwaki S, Noda A, Cullings HM, Macphee DG, et al. Heterozygous individuals bearing a founder mutation in the XPA DNA repair gene comprise nearly 1% of the Japanese population. Mutat Res 2006 Oct;601(1-2):171-178.
7. Bhutto AM, Shaikh A, Nonaka S. Incidence of xeroderma pigmentosum in Larkana, Pakistan: a 7-year study. Br J Dermatol 2005 Mar;152(3):545-551.
8. Stary A, Sarasin A. The genetics of the hereditary xeroderma pigmentosum syndrome. Biochimie 2002 Jan;84(1):49-60.
9. Eugene DW, Joshi KD. Xeroderma pigmentosa–a disfiguring disease. Kathmandu Univ Med J (KUMJ) 2006 Jan-Mar;4(1):78-81.
10. Patil MR, Vishwanath V, Arya M, Shenoy BP, Bharmal RN, Torsekar RG. Pilomatricoma in a case of familial xeroderma pigmentosum. Indian J Dermatol Venereol Leprol 2007 May-Jun;73(3):198-199.
11. El-Hayek M, Lestringant GG, Frossard PM. Xeroderma pigmentosum in four siblings with three different types of malignancies simultaneously in one. J Pediatr Hematol Oncol 2004 Aug;26(8):473-475.
12. Green WH, Wang SQ, Cognetta AB Jr. Total-body cutaneous examination, total-body photography, and dermoscopy in the care of a patient with xeroderma pigmentosum and multiple melanomas. Arch Dermatol 2009 Aug;145(8):910-915.
13. Mohanty P, Mohanty L, Devi BP. Multiple cutaneous malignancies in xeroderma pigmentosum. Indian J Dermatol Venereol Leprol 2001 Mar-Apr;67(2):96-97.
14. Masinjila H, Arnbjörnsson E. Two children with xeroderma pigmentosum developing two different types of malignancies simultaneously. Pediatr Surg Int 1998 Apr;13(4):299-300.
|