|
Introduction
Hearing loss is a known complication of viral infections such as coxsackievirus, cytomegalovirus, herpes, influenza, measles, and mumps. These etiologies most commonly produce sensory neural hearing loss. Pathogenetically, their hearing loss is related to acoustic neuritis with fibrosis for measles and direct viruses -induced cytolysis by atrophy of the corti organ for mump viruses.1-3
Hearing loss due to viral infection can be unilateral or bilateral, and ranges from partial to severe hearing loss that will often be permanent.4 Viral hepatitis has been shown to be associated with various extrahepatic manifestations. Its otologic manifestations are similar as well. Polyarteritis nodosa is a life threatening necrotizing vasculitis that affects medium-sized arteries, and its association with hepatitis B virus is well-documented. Hearing loss may be the presenting symptom of this disease.5,6 Hepatitis B has multisystem complication and the involvement of the inner ear in hepatitis B is reported in the literature to potentially cause deafness.7 Thus, hearing loss in patients with positive hepatitis B is studied.
Methods
One hundred consecutive patients with hepatitis B (HBS-Ag positive) between August 2005 and October 2009 were chosen for this study. The patients were compared with one hundred cases who had undergone hepatitis B examination as the control group. These two groups underwent complete clinical history, physical and audiologic examinations. All the cases in control group were HBS-Ag negative. Cases with history of trauma to the ear or skull, ear infection or tumors, autoimmune diseases and other known etiology hearing loss were excluded from both groups. Pure-tone audiometry (PTA) and pure tone average of the right and left ears (average between 250, 500, 1000, 2000, 4000 and 8000 Hz) along with speech discrimination score (SDS) were performed for the two groups by a professional audiologist using AC 40, Interacostics, Assen, Danmark. Also, tympanometry was performed to evaluate the acoustic reflex by Amplaid 775, Milan, Italy. The audiometry and tympanometry equipment were calibrated in the last 6 months. Audiological assessment was performed before starting any medical treatment for hepatitis B patients (newly diagnosed as HBS-Ag positive) and hearing loss was considered if the threshold was more than 20 dB.
Statistical analysis was done using SPSS 16.0 for windows and a p-value of <0.05 was considered statistically significant. This study was directly reviewed and approved by the ethics committee at Hamedan University of Medical Sciences.
Results
Five patients and three control cases were excluded because of ear trauma or disease. Ninety-five patients and 97 non-hepatic B (negative HBS-Ag) cases were enrolled in the study. The mean age was 36.3±7.4 years in the patient group and 33.4±12.5 years in the control group. Male-to-female ratio in the patient group was 7 to 3 and 7.5 to 2.5 in the control group. There were no statistical difference in age and sex between the two groups.
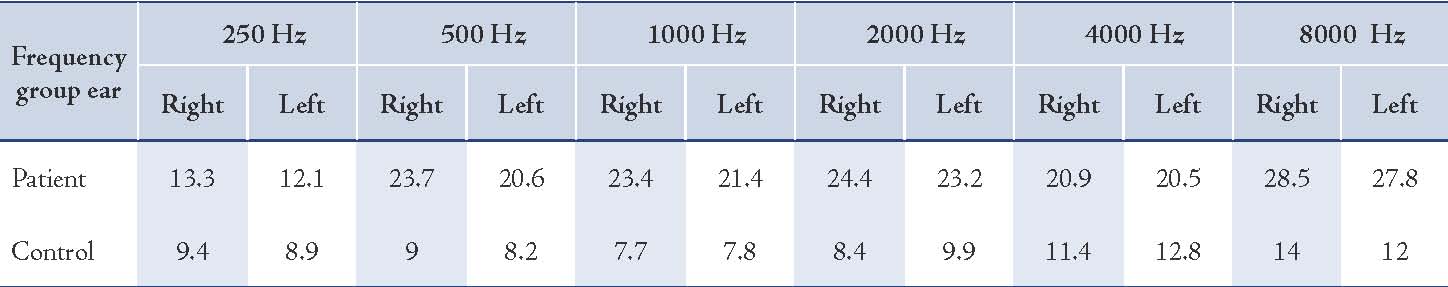
Pure tone average (mean thresholds 500, 1000 and 2000 Hz) was 22.1 dB in the left and 23.95 dB in the right ear (hearing loss). In the control group, PTA average was 8.4dB in the left and 8.95 dB in the right ear (normal hearing). In both groups, SDS was 100% in both ears. There was no significant difference in both ears (p>0.1 [Table 1]). The considered average thresholds in both ears were shown in Fig. 1. The acoustic reflex thresholds and SDS were normal in both ears for the patient and control groups. Average pure tone of the two groups exhibited a significant difference (p=0.01) as shown in Table 2. There was no marked pattern for hearing loss in the patient group, although losses were frequently asymmetric.
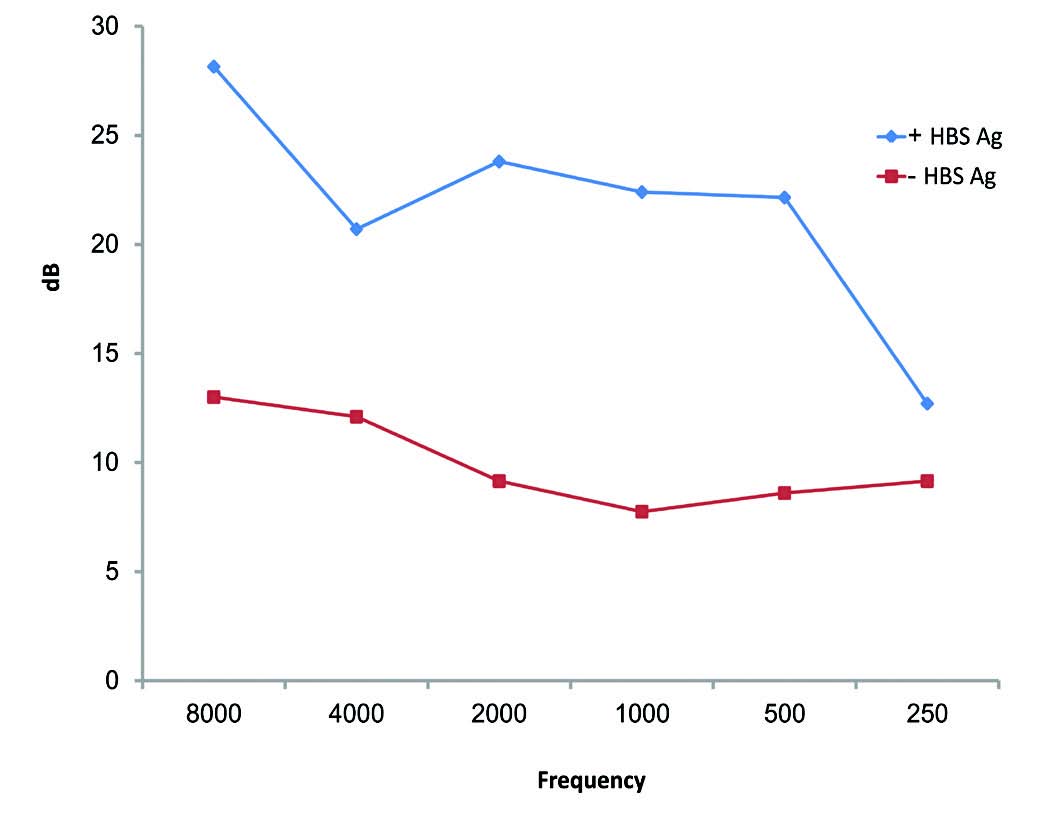
Figure 1: Mean Frequency-specific results in PTA (dB) of the patients with hepatitis B (+HBS-Ag) and the control groups (-HBS Ag) considering the average thresholds in both ears.
Table 1: Mean pure tone average (dB) results of the patients with hepatitis B and control groups.
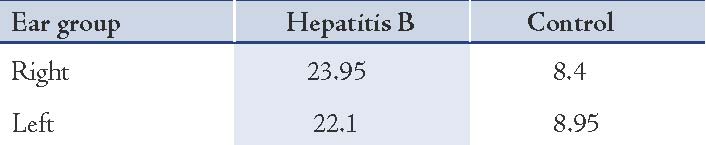
Table 2: Mean frequency-specific results in PTA (dB) of the patients with hepatitis B and the control groups.
Discussion
The known etiologies of acquired sensorineural hearing loss include acoustic trauma, physical trauma, ototoxicity, genetic predisposition, infections, Meniere’s disease, aging, and autoimmune diseases. Autoimmune inner ear disease was first described in 1979 and the disease has become more widely recognized over the last decade. Autoimmune inner ear disease is not a uniform disease with simple diagnosis and treatment.8 Viruses such as parvovirus B19 can be a possible etiology of autoimmune inner ear disease.9 Polyarteritis nodosa is a systemic disease which affects the small- to medium-sized muscular arteries. Sudden or progressive hearing loss is one of the otologic manifestations of an immune-mediated inner ear disease in polyarteritis nodosa.10 The presence of hepatitis B antigenemia (HBS-Ag) in approximately 30% of patients with polyarteritis nodosa, as well as immune complexes of HBS-Ag immunoglobulin and complement in blood vessel walls strongly suggest the role of immunologic phenomena.11
Polyarteritis nodosa is one of the common forms of vasculitis with multiorgan involvement. Hearing loss may be the presenting symptom of this disease. Systemic vasculitis such as polyarteritis nodosa may rarely result in a rapidly progressive hearing loss. Although deafness is recognized as being associated with it, rarely is hearing loss a herald of polyarteritis nodosa.6,12 In this disease, temporal bone findings have shown the relationship between sensorineural hearing loss and labyrinthine vasculitis.13 Constellation of symptoms may occur as a primary disorder in polyarteritis nodosa.14 If hepatitis B relates to polyarteritis nodosa, the inner ear could be affected by underlying systemic immune dysfunction. In this study, none of the patients had polyarteritis nodosa, vaccination for hepatitis B, or any treatment for hepatitis that affect their hearing thresholds. This means that hepatitis B alone can affect hearing threshold by inner ear involvement although none of the patients had conventional hearing loss (>30 dB). In this study, SDS in the audiometric test did not show retrocochlear involvement, but auditory brainstem response (ABR) assessment would have helped to distinguish not only the central pathways but also the brainstem neural integrity.15 Therefore, future direction of study should be to assess the HBS-Ag positive patients with ABR, otoacoustic emission (OAE), and electrocochleography (ECOG) testing for better evaluation of the inner ear, cochlear nerve, brain stem and cerebral neural pathways.
Conclusion
The present study demonstrates the association between hepatitis B and sensorineural hearing loss (SNHL) and a need is felt to conduct further studies involving the temporal bones in hepatitis-B patients. It is suggested that physicians ask for HBS-Ag test for the presence of hepatitis B in patients with bilateral SNHL with unknown etiology, and be aware that hepatitis B prophylaxis is valuable in decreasing hepatitis B involvement and therefore hearing loss.
Acknowledgements
The authors reported no conflict of interest and no funding was received in this work.
References
1. Mishra B, Panda N, Singh MP, Ratho RK. Viral infections in sudden hearing loss. Do we have enough evidence? Kathmandu Univ Med J (KUMJ) 2005 Jul-Sep;3(3):230-233. KUMJ.
2. Noorbakhsh S, Farhadi M, Tabatabaei A, Mohamadi S, Jomeh E. Infection in childhood sensory hearing loss. Saudi Med J 2008 Oct;29(10):1470-1474.
3. Greco A, Fusconi M, Gallo A, Marinelli C, Macri GF, De Vincentiis M. Sudden sensorineural hearing loss: an autoimmune disease? Autoimmun Rev 2011 Oct;10(12):756-761. Published online 18 May 2011.
4. Tsubota M, Shojaku H, Ishimaru H, Fujisaka M, Watanabe Y. Mumps virus may damage the vestibular nerve as well as the inner ear. Acta Otolaryngol 2008 Jun;128(6):644-647.
5. Janssen HL, van Zonneveld M, van Nunen AB, Niesters HG, Schalm SW, de Man RA. Polyarteritis nodosa associated with hepatitis B virus infection. The role of antiviral treatment and mutations in the hepatitis B virus genome. Eur J Gastroenterol Hepatol 2004 Aug;16(8):801-807.
6. Joglekar S, Deroee AF, Morita N, Cureoglu S, Schachern PA, Paparella M. Polyarteritis nodosa: a human temporal bone study. Am J Otolaryngol 2010 Jul-Aug;31(4):221-225. Published online 17 May 2009.
7. Huang CC, Lin WB, Chang PH, Chan KC, Lee TJ. Sudden deafness as a presenting symptom of chronic hepatitis B with acute exacerbation. Otolaryngol Head Neck Surg 2009 Nov;141(5):659-660.
8. Broughton SS, Meyerhoff WE, Cohen SB. Immune-mediated inner ear disease: 10-year experience. Semin Arthritis Rheum 2004 Oct;34(2):544-548.
9. Nara M, Shirata Y, Kikuchi T, Hongo M. Tohoku. Adult human parvovirus-B19 infection presenting with hearing difficulty and dizziness. J Exp Med 2011;224(1):57-59.
10. Stone JH,Francis HW.Immune-mediated inner ear disease. Curr Opin rheumandol Jun 2000;12(1):32-40.
11. Choucair J, Hajj G, Abi Karam G. A case of PAN with positive Hbs Ag cured by immunosuppressive and antiviral therapies: a case report. J Med Liban 2007 Jan-Mar;55(1):50-52.
12. Tsunoda K, Akaogi J, Ohya N, Murofushi T. Sensorineural hearing loss as the initial manifestation of polyarteritis nodosa. J Laryngol Otol 2001 Apr;115(4):311-312.
13. Joglekar S, Deroee AF, Morita N, Cureoglu S, Schachern PA, Paparella M. Polyarteritis nodosa: a human temporal bone study. Am J Otolaryngol 2010 Jul-Aug;31(4):221-225.
14. Psillas G, Kyriafinis G, Daniilidis J. Polyarteritis nodosa and cochlear implantation. J Laryngol Otol 2007 Feb;121(2):196-199.
15. Bayazit Y, Yilmaz M, Kepekçi Y, Mumbuç S, Kanlikama M. Use of the auditory brainstem response testing in the clinical evaluation of the patients with diabetes mellitus. J Neurol Sci 2000 Dec;181(1-2):29-32.
|