Tuberculous adenitis, the most common form of tuberculosis (TB), is one of the most frequently occurring infectious diseases worldwide. It accounts for between 2% and 5% of all TB cases and is more common among children and immunosuppressed patients, especially those with HIV.1,2 It comprises 43.5% of extrapulmonary TB cases in Qatar.3 Lymphomas may occasionally mask TB adenitis, particularly in patients with predominant systemic symptoms such as fever, night sweats, and weight loss. However, the concomitant occurrence of TB adenitis and Hodgkin lymphoma (HL) is rare, as evidenced by the scarcity of cases reported in the literature.
We report this case intending to increase physicians’ awareness of the simultaneous occurrence of these two conditions particularly when they encounter initial therapeutic failure during the treatment of HL or tuberculous adenitis.
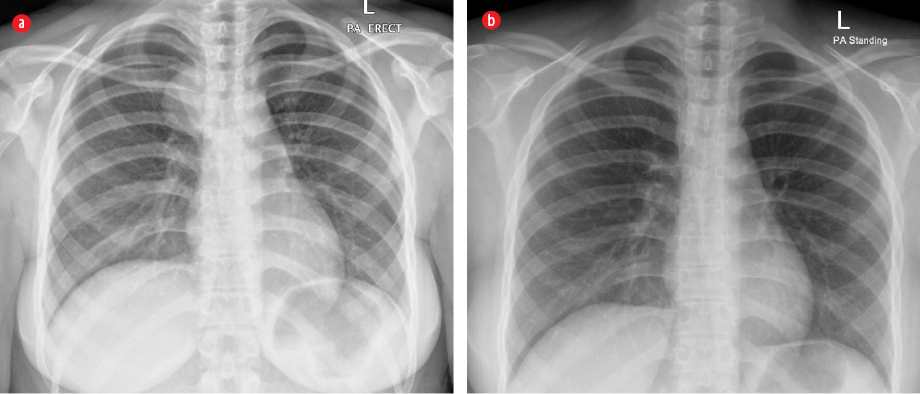
Figure 1: (a) Presence of a right para-tracheal circumscribed mass. (b) The mass was absent after
treatment completion.

Figure 2: Contrast-enhanced CT of the neck showed an amalgamated mass lesion in the supraclavicular regions bilaterally.

Figure 3: Contrast-enhanced CT of the thorax and abdomen showed multiple enlarged lymph nodes in the base of the neck, mediastinum, and retroperitoneum region.
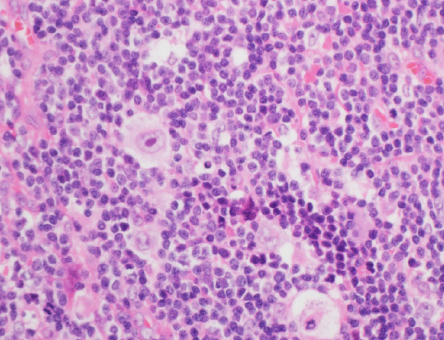
Figure 4: Lymph node biopsy revealing the presence of Reed-Sternberg cells. Hematoxylin and eosin staining, magnification = 200 ×.
Case Report
A 15-year-old girl, previously healthy, presented to our hospital with a three-month-history of progressive and painless right neck swelling. She also reported having low-grade fever, weight loss of 6 kg, generalized fatigue, and dry cough for the same period. Her medical history was unremarkable, and there was no history of contact with any sick person. Physical examination was only remarkable for a 5 × 5 cm, hard, non-tender, and matted right supraclavicular lymphadenopathy. Her laboratory workup were only significant for elevated lactic acid dehydrogenase (LDH = 347 U/L) and mild microcytic anemia (hemoglobin = 10.4 gm/dL). Chest X-ray showed a right para-tracheal circumscribed mass [Figure 1a]. Contrast-enhanced computer tomography (CT) of the neck showed an amalgamated mass lesion in the supraclavicular regions bilaterally (more on the right and in the superior mediastinum), while contrast-enhanced CT of the chest and abdomen showed multiple enlarged lymph nodes in the base of the neck, mediastinum, and retroperitoneum regions [Figure 2 and 3]. Purified protein derivative testing was positive (16 mm after 24 hours).
Fine needle aspiration (FNA) from the right supraclavicular lymph node revealed occasional large lymphoid-like cells, approximately 10-times larger than normal lymphocytes, and occasionally bi-lobed forms, suspicious for lymphoma. Samples of FNA also were sent for acid-fast bacilli (AFB) smear, TB-polymerase chain reaction (TB-PCR), and mycobacterial culture. As the FNA was suspicious for lymphoma, an excisional biopsy was performed on the same lymph node, and histopathological examination revealed small lymphocytes admixed with large atypical cells, including Reed-Sternberg cells and other Hodgkin cells, consistent with classical HL of lymphocyte-rich subtype [Figure 4].
Immunohistochemistry showed strong reaction to CD15 and CD30, and was negative for CD45. Alongside, the FNA samples showed positive results for PCR and AFB and later confirmed by cultures as Mycobacterium tuberculosis.
The patient was diagnosed with HL and tuberculous adenitis and was started on anti-tubercular drugs as well as on chemotherapy. She received four-drug anti-tuberculous therapy (isoniazid, rifampicin, pyrazinamide, and ethambutol) for six months. In addition, she received two cycles of OEPA (vincristine, etoposide, prednisone, and doxorubicin), followed by four cycles of COPDAC (cyclophosphamide, vincristine, prednisone, and dacarbazine) as HL treatment. The patient showed good tolerance to chemotherapy and anti-tubercular drugs. The fever subsided after two weeks, and the neck lymph nodes became unpalpable after three cycles of chemotherapy. Upon completion of therapy, follow-up chest X-ray revealed the absence of right para-tracheal circumscribed mass [Figure 1b] and the whole-body fluorodeoxyglucose-positron emission tomography scan showed no obvious uptake in previously affected lymph nodes and bone involvements indicating complete remission of the disease.
Discussion
The association between tuberculous adenitis and HL has been discussed since the diagnosis of Hodgkin disease. The essence of this discussion was whether or not HL is a form of TB. Finally, it was concluded that HL is an independent entity, but sometimes associated with TB.4 This association is rare, and only six reported cases were found.5–9 To the best of our knowledge, this is the first case reported in Qatar. Table 1 describes the clinical aspects of the six reported cases as well as ours.
As shown in Table 1, tuberculous adenitis and HL can co-occur at any age and in both sexes, with fever being the most common symptom. The diagnosis of HL was delayed in cases 1, 2, 3, and 5 as the initial diagnosis was tuberculosis adenitis, and the patients were started on anti-TB medications, but did not improve. The reasons for re-investigating these cases are mentioned in Table 1, which showed that the simultaneous occurrence of these entities was missed and only noticed when there was relapse or failure in treatment of one of them.
Table 1: Clinical characteristics of the reported cases of concurrent tuberculous adenitis and HL.
|
1 |
Bonadonna,4 |
40/M
49/F |
Fever and LAD
Anorexia, weight loss, fever, HSM, LAD |
Tuberculous adenitis
Tuberculous adenitis |
LN size unchanged
Relapse of fever |
Axillary and mediastinum
Same inguinal LN |
Nodular sclerosis
Nodular sclerosis |
Cured
Cured |
|
2 |
Costa et al,5 |
29/F |
Cough, hemoptysis, SOB, chest pain, LAD |
Tuberculous adenitis |
LN size increased |
Cervical and mediastinum |
Nodular sclerosis |
Cured |
|
3 |
Reddy et al,6 |
18/M |
Anorexia, fever, HSM, LAD |
HL and tuberculous adenitis |
Incidental finding |
Same cervical LN |
Mixed cellularity |
Cured |
|
4 |
Mahajan
et al,7 |
71/F |
Fatigue and LAD |
Tuberculous adenitis |
LN size increased |
Same axillary LN |
Lymphocytic predominant |
Cured |
|
5 |
Ban et al,8 |
52/M |
Fatigue, SOB, cough, weight loss, night sweats, fever, LAD |
HL and tuberculous adenitis |
Incidental finding |
Same cervical LN |
Lymphocytic predominant |
Unknown |
LN: lymph node; HL: Hodgkin lymphoma; F: female; M: male; HSM: hepatosplenomegaly; LAD: lymphadenopathy; SOB: shortness of breath.
If the diagnosis of one of these conditions is missed initially, this may affect the outcome. As noted in case 2, the initial response to anti-TB therapy masked and delayed the diagnosis, which may affect the stage and, therefore, the prognosis of HL, but the patient was lucky because this was not the case. In cases 3 and 5, the increase in lymph nodes size may be considered by some physicians as a paradoxical reaction during TB treatment, and they may attempt a short course of steroids that will increasingly mask the HL and may lead to serious complications. The other scenario that fortunately did not happen, what would happen if HL is diagnosed and TB is missed? The initiation of chemotherapy could cause life-threatening dissemination of TB.
Concurrent occurrence of HL and tuberculous adenitis poses a unique challenge for clinicians in terms of management and prognosis since, apart from scarce case reports, no large therapeutic studies have been conducted. However, the response to treatment and the prognosis seems to be good considering six patients were cured [Table 1].
Two theories have been proposed to explain the concomitant occurrence of TB lymphadenitis and HL. The first stated that having a malignancy like HL can suppress the cell-mediated immunity, which in turn can lead to activation of TB.10 The second proposed that mycobacterium TB infection can cause direct DNA damage and apoptosis inhibition, which can lead to mutations and predispose to malignancies such as lymphoma.11,12
Conclusion
The concomitant onset of tuberculous adenitis and HL is rare, and a high index of clinical suspicion is needed to avoid missing the diagnosis. Hence, physicians’ should consider the occurrence of both conditions simultaneously when they encounter initial therapeutic failure during the treatment of HL or tuberculous adenitis.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Gerogianni I, Papala M, Kostikas K, Ioannou M, Karadonta AV, Gourgoulianis K. Tuberculous disseminated lymphadenopathy in an immunocompetent non-HIV patient: a case report. J Med Case Rep 2009 Dec;3:9316.
- 2. Muluye D, Biadgo B, Woldegerima E, Ambachew A. Prevalence of tuberculous lymphadenitis in Gondar University Hospital, Northwest Ethiopia. BMC Public Health 2013 May;13:435.
- 3. Khattab MA, Khan FY, Maslamani MA, Al-Khal AL, Gendy AE, Soub HA, et al. Pulmonary and extra pulmonary tuberculosis in Qatar: a first retrospective population-based study. Adv Infect Dis 2015;05:148-153.
- 4. Bonadonna G. Historical review of Hodgkin’s disease. Br J Haematol 2000 Sep;110(3):504-511.
- 5. Costa LJ, Gallafrio CT, França FO, del Giglio A. Simultaneous occurrence of Hodgkin disease and tuberculosis: report of three cases. South Med J 2004 Jul;97(7):696-698.
- 6. Reddy RC, Mathew M, Parameswaran A, Narasimhan R. A case of concomitant Hodgkin’s lymphoma with tuberculosis. Lung India 2014 Jan;31(1):59-62.
- 7. Mahajan K, Gupta G, Singh DP, Mahajan A. Simultaneous occurrence of ’Hodgkin’s disease and tubercular lymphadenitis in the same cervical lymph node: a rare presentation. BMJ Case Rep 2016;2016.
- 8. Ban WH, Kang HH, Baeg MK, Kim JG, Kim HJ, Baek IW, et al. Coexistence of Hodgkin’s lymphoma and tuberculosis in the same axillary lymph nodes. Tuberc Respir Dis (Seoul) 2011;70:342-346.
- 9. Valchev D, Mitev M, Obretenov E, Kostadinov D, Petrov D. A Combination of Hodgkin’s lymphoma and tuberculosis occurred with bilateral malignant pleural effusions. Ann Case Rep 2018: ACRT-169.
- 10. Karakas Z, Agaoglu L, Taravari B, Saribeyoglu E, Somer A, Guler N, et al. Pulmonary tuberculosis in children with Hodgkin’s lymphoma. Hematol J 2003;4(1):78-81.
- 11. Kumar P, Verma A, Saini AK, Chopra P, Chakraborti PK, Singh Y, et al. Nucleoside diphosphate kinase from Mycobacterium tuberculosis cleaves single strand DNA within the human c-myc promoter in an enzyme-catalyzed reaction. Nucleic Acids Res 2005 May;33(8):2707-2714.
- 12. Sachdev R, Duggal R, Agrawal K, Goel S. Coexistent nodal diffuse large B-cell lymphoma with extrapulmonary tuberculosis: a rare case. Int J Surg Pathol 2016 Feb;24(1):
70-72.