Pilomatricoma is an uncommon benign skin tumor arising from the hair follicle. It is usually found in the head and neck regions and is typically seen in the pediatric age group particularly girls. Clinical characterization may be difficult, and it can be easily misdiagnosed as a malignant tumor of parotid origin in the setting of preauricular swelling. Clinicians should consider this benign neoplasm in the differential diagnosis of preauricular swelling and pediatric neck masses.

Figure 1: (a) Preoperative lateral view of a preauricular mass mimicking a parotid tumor. (b) Cosmetic outcome one-month postoperatively demonstrating excellent wound healing.
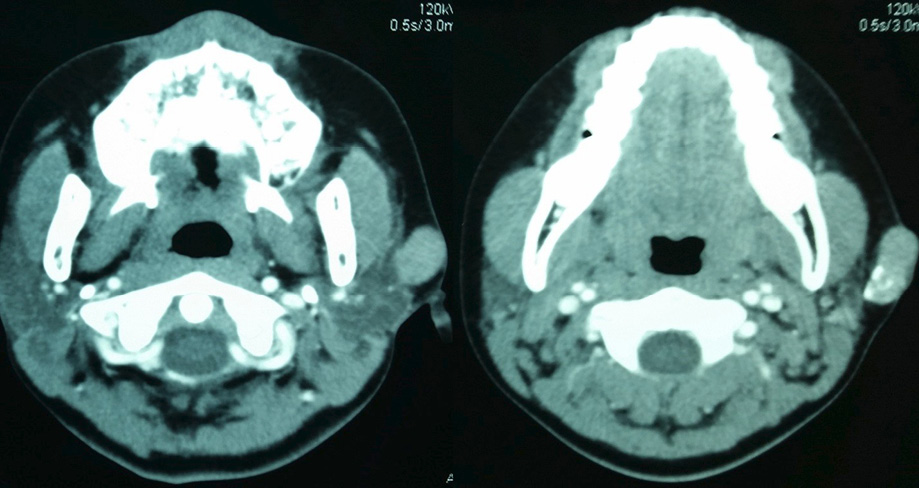
Figure 2: Contrast enhanced computed tomography scan showed well-defined lobulated lesion with coarse calcification arising from the skin/subcutaneous tissue with suspicious parotid involvement.

Figure 3: Gross tumor specimen demonstrating a hard, irregular mass with white-yellowish color.
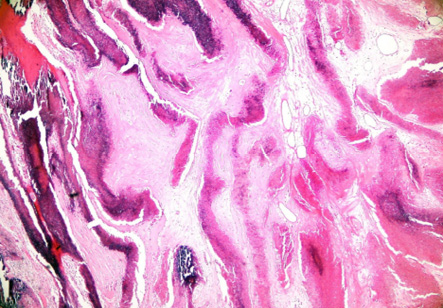
Figure 4: Photomicrograph of the excised specimen showing solid nests of basaloid cells undergoing abrupt keratinization forming nests of pinkish ghost cells diagnostic of pilomatricoma. Hematoxylin and eosin staining, magnification = 4 ×.
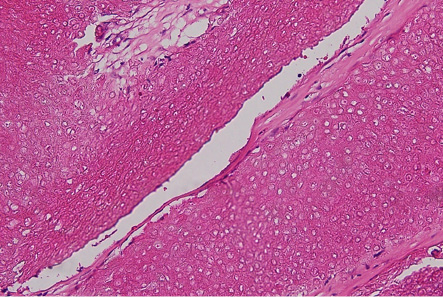
Figure 5: Sheets of ghost cells seen exhibiting only the basic cellular outline but lacking nuclear and cytoplasmic details. Hematoxylin and eosin staining, magnification = 40 ×.
Case report
A 12-year-old girl presented with a left preauricular swelling present for the last two years, which became progressively larger and more painful in the weeks before presentation. On examination, the mass was mildly tender, and had an irregular stony-hard surface with overlying reddish skin discoloration [Figure 1]. It was ill-defined with restricted mobility to the skin and deeper structures. There was no facial nerve dysfunction. Due to its malignant-appearing clinical presentation, the swelling was thought to be arising from the left parotid gland. Multiple attempts of fine-needle aspiration cytology (FNAC) were inconclusive. Computed tomography (CT) scan eventually showed a well-defined calcified subcutaneous mass with suspicious involvement of the parotid gland [Figure 2]. The case was posted for tumor excision and superficial parotidectomy. Intraoperatively, however, this lesion was confined to the subcutaneous space and could be easily separated from the parotid gland, which was left intact. The lesion was excised with its capsule [Figure 3] and the overlying skin was then repaired with primary closure. Histopathological examination of the excised specimen confirmed a typical pilomatricoma, which showed characteristic ghost cells, basophilic cells, and ossifications [Figure 4 and 5]. There were also abrupt and gradual transitions of the basaloid cells to squamous and ghost cells. Her postoperative course
was uneventful.
Discussion
Pilomatricoma (formerly known as pilomatrixoma or calcifying epithelioma of Malherbe) is a benign calcifying tumor arising from the hair matrices with the cheek and preauricular regions being the most frequently affected sites.1–6 It has a predilection for females (male to female ratio of 1:1.5) and tend to occur in children.1–6 Clinical presentation is variable but it typically presents as a slow growing, superficial, mobile, stony-hard mass with bluish or reddish discoloration. It is usually solitary, but up to 10% may present as multiple tumors and the latter may be associated with Gardner syndrome, myotonic dystrophy, or Turner’s syndrome.1,2
Fifty-five percent of lesions present as stony-hard masses, 74% are fixed to the skin, 96% range from 0.5 cm to 5 cm in size, 42% have progressive enlargement, and only 34% have normal overlying skin.3 Some lesions are pedunculated with surface ulcerations and redness.7 As a result of this seemingly inconsistent clinical features, pilomatricoma has been found to be one of the most frequent mimicker of salivary gland tumors.5
The diagnosis of pilomatricoma is usually suspected clinically and confirmed by histopathological examination. Preoperative imaging is rarely indicated unless its presentation poses a diagnostic dilemma, such as in our case when misdiagnosis of a primary malignant parotid tumor was made followed by multiple inconclusive FNACs. CT scan or magnetic resonance imaging can help in defining its location and its relation to the parotid gland. FNAC can be inconclusive even after several attempts (three in total for our patient) and may potentially be misleading in the event of incorrect diagnosis of a malignant tumor.1,5 Since pilomatricoma does not spontaneously regress, complete excision of the lesion along with clear margins is recommended as it is both diagnostic and curative.1–5
Typical histopathological findings show cells in dermal nodules arranged in a circular configuration, with nucleated basaloid cells on the periphery, and enucleated shadow (ghost) cells with calcifications in the center [Figure 4 and 5].5 Cytologically, it can be misdiagnosed as a malignancy when basaloid cells predominate the aspirate, more so in the absence of ghost cells.4 Recurrences and malignant transformations are rare.1–5
Our case demonstrates a rare benign tumor mimicking an aggressive parotid mass at initial presentation. Retrospectively, there were some typical features of this tumor including the age of a female patient below 20 years, a solitary slow growing stony-hard mass fixed to the overlying skin, and reddish skin discoloration. However, we could not distinguish this benign entity from that of a malignant parotid tumor with skin involvement clinically. CT scan showed a predominant subcutaneous mass but with features of suspicious parotid involvement. Preoperative managements were inconclusive and offered no symptomatic relief, so we opted for total excision in pursuit of a definitive diagnosis.
Conclusion
Pilomatricomas at the preauricular region may pose as diagnostic dilemmas. A heightened knowledge of the disease is needed for early recognition of clinical and imaging features to prevent aggressive therapy than is required for these benign hair
follicle neoplasms.
Disclosure
The authors declared no conflicts of interest.
references
- 1. Agarwal RP, Handler SD, Matthews MR, Carpentieri D. Pilomatrixoma of the head and neck in children. Otolaryngol Head Neck Surg 2001 Nov;125(5):510-515.
- 2. O’Connor N, Patel M, Umar T, Macpherson DW, Ethunandan M. Head and neck pilomatricoma: an analysis of 201 cases. Br J Oral Maxillofac Surg 2011 Jul;49(5):354-358.
- 3. Yoshimura Y, Obara S, Mikami T, Matsuda S. Calcifying epithelioma (pilomatrixoma) of the head and neck: analysis of 37 cases. Br J Oral Maxillofac Surg 1997 Dec;35(6):429-432.
- 4. Yencha MW. Head and neck pilomatricoma in the pediatric age group: a retrospective study and literature review. Int J Pediatr Otorhinolaryngol 2001 Feb;57(2):123-128.
- 5. Cozzi DA, d’Ambrosio G, Cirigliano E, Negro V, Iacusso C, Totonelli G, et al. Giant pilomatricoma mimicking a malignant parotid mass. J Pediatr Surg 2011 Sep;46(9):1855-1858.
- 6. Bozkurt P, Kolsuz ME, Günhan Ö, Erdem E, Orhan K. Preauricular pilomatricoma: An uncommon entity in a dental pediatric patient. Int J Surg Case Rep 2017;30:62-65.
- 7. Inamura Y, Hata H, Imafuku K, Kitamura S, Shimizu H. Would you consider pilomatricoma as a differential diagnosis? Our Dermatol Online 2016;7(1):117-118.