A62-year-old female presented with a three-day history of painful purple-red nodules on her face and extremities [Figure 1] associated with generalized malaise and arthralgia. The patient had a significant medical history of monoclonal gammopathy of undetermined significance diagnosed in 2008, ovarian cancer, which was treated with surgery and chemotherapy in 2010, and thyroid cancer for which she underwent a thyroidectomy in 2011.
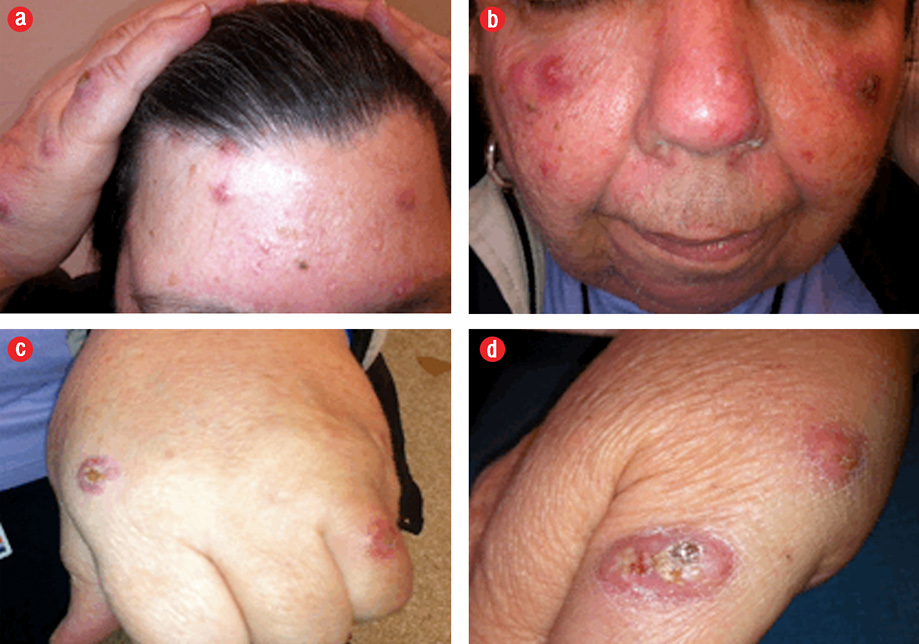
Figure 1: Erythematous, tender nodules, and papules, some with central crusting distributed asymmetrically over the face, dorsum hands, arms, and thighs.
Laboratory investigations showed normal complete blood counts, high C-reactive protein levels (27.4 mg/L; normal range 0–5 mg/L), normal renal and liver function, normal CA 125 level, and normal bone marrow biopsy. Serum protein electrophoresis showed monoclonal immunoglobulin (Ig)-A with lambda peak. A skin biopsy revealed diffuse neutrophilic dermatitis with no evidence of vasculitis or stainable microorganisms.
Questions
- What is the diagnosis?
a. Sweet’s syndrome
b. Leukaemia cutis
c. Neutrophilic eccrine hidradenitis
- Is there any association between monoclonal gammopathy of undetermined significance and this condition?
a. Yes
b. No
- What is the first-line treatment?
a. Systemic corticosteroid treatment
d. Ciclosporin
c. Thalidomide
Answers
- Sweet’s syndrome.
- Yes. There are few case reports describing the associations between monoclonal gammopathy of undetermined significance and sweet’s syndrome.
- The gold standard treatment is the use of systemic corticosteroids. Other first-line oral systemic agents are potassium iodide and colchicine. Second-line oral systemic agents include indomethacin, clofazimine, ciclosporin, and dapsone.
Discussion
Robert Douglas Sweet originally described Sweet’s syndrome in 1964 as an acute febrile neutrophilic dermatosis.1 The syndrome is considered a reactive neutrophilic dermatosis to a wide range of underlying or preceding conditions, including viral illnesses, inflammatory bowel disease, malignancies, and drug exposure. It is characterized by clinical, pathological, and laboratory findings, which include pyrexia, neutrophilia, tender erythematous skin lesions (papules, nodules, and plaques), and a diffuse infiltrate consisting predominantly of mature neutrophils that are typically located in the upper dermis. Sweet’s syndrome can also present with extracutaneous manifestations that affect the bones, central nervous system, eyes, kidneys, gastrointestinal tract, heart, and lungs.1
Sweet’s syndrome can also be classified based on the clinical setting in which it occurs: classical or idiopathic, malignancy-associated, and drug-induced. The classical or idiopathic Sweet’s syndrome usually presents in women between the age of 30 to 50 years and may be associated with infection of the upper respiratory tract or gastrointestinal tract, inflammatory bowel disease, and/or pregnancy. Malignancy-associated Sweet’s syndrome can occur as a paraneoplastic syndrome in patients with an established or undiscovered hematological malignancy or solid organ tumor. The most common hematologic disorders associated with Sweet’s syndrome are acute myelogenous leukemia, myelodysplastic syndromes and chronic myelogenous leukemia.2 Carcinomas of the genitourinary organs, breast, and gastrointestinal tract are the most frequently occurring cancers in patients with Sweet’s syndrome with solid tumors.2 The most frequent medication associated with drug-induced Sweet’s syndrome is granulocyte-colony stimulating factor.3 However, several other medications have been observed to promote the development of Sweet’s syndrome such as minocycline, trimethoprim-sulfamethoxazole, retinoids, and contraceptive pills.1
Sweet’s syndrome has been reported in association with monoclonal gammopathy of undetermined significance (MGUS) and multiple myeloma.4 MGUS is defined as a serum M protein level of less than 3 g/dL, less than 10% clonal plasma cells in the bone marrow, and the absence of end-organ damage.5 MGUS may progress to multiple myeloma, amyloid light-chain (AL) amyloidosis, Waldenström macroglobulinemia, or lymphoma. It is recommended to include immunoelectrophoresis to be part of the work-up of all patients with Sweet’s syndrome because of the high association with malignancy, in particular, hematologic diseases, and the fatal outcome in some of the reported cases.
The therapeutic gold standard for Sweet’s syndrome is systemic corticosteroids, which when administered result in a prompt response improving both the dermatosis-related symptoms and skin lesions.4 Topical application of high potency corticosteroids or intralesional corticosteroids may be effective for treating localized lesions. Other first-line oral systemic agents are potassium iodide and colchicines.6 Second-line oral systemic agents include indomethacin, clofazimine, ciclosporin, and dapsone.6
references
- 002;3(2):117-131.