|
Introduction
Traumatic aortic injuries are not uncommon. Ninety percent of traumatic aortic injuries result from penetrating causes such as gunshot or stab wounds, with only 10% being due to blunt thoracic trauma.1 About 70% to 90% of blunt aortic injuries are caused by automobile accidents. Blunt aortic injuries are rapidly lethal in 90% of cases due to transection, rupture, and exsanguination, with survivors having a contained aortic leak leading to pseudo aneurysms, intramural hematoma, dissection, thrombus, or hemomediastinum. We present a patient with left hemiplegia secondary to Stanford type A aortic dissection extending to the supra-aortic vessels, which was precipitated by the recoil of a rifle butt.
Case report
A 59-year-old male, non-hypertensive, non-diabetic with no past medical problems presented with history of left hemiplegia. While holidaying in Kenya, on a hunting spree utilizing rifles, he developed a sudden onset of severe low backache with transient weakness of the left arm recovering within a few hours. He did not have anterior chest or interscapular pain. He was seen by a general practitioner and an orthopaedician who advised a lumbar belt. After 2 weeks, he returned to Oman and presented to a hospital with recurrence of left arm and leg weakness. He was diagnosed to have right common carotid artery thrombus by carotid duplex ultrasonography and was started on warfarin and discharged. His weakness persisted over a week and he visited the emergency department at Royal Hospital, Oman.
On examination, he was alert and fully orientated; blood pressure was 150/60 mmHg in the left arm and 140/60 mmHg in the right arm. He did not have features of marfan syndrome. Neurological examination had revealed left side hemiplegia (Medical Research Council grade 3/5 power) with left upper motor neuron facial palsy, mild dysphasia with intact cranial nerves. Cardiovascular examination revealed equal peripheral pulses with no bruit, but an early diastolic murmur was heard in the right second intercostal space. He was admitted to the neurology ward for further workup. An echocardiogram was requested to rule out significant valvular disease or any thrombus.
Transthoracic echocardiogram showed a dilated aortic root measuring 5.2 cm with a spiral aortic dissection (AoD) (Fig. 1A). An intimal flap divided the aortic channel into false and true lumens (Fig. 1B), which was confirmed by computed tomography (CT) of the chest and abdomen. The dissection flap extended to the arch of aorta, innominate artery and right common carotid arteries (Fig. 1C), as well as the descending aorta reaching up to the left iliac artery (Fig. 2A). There was moderate to severe aortic regurgitation and mild pericardial effusion. On enquiry, the patient denied any history of automobile accident or fall, but recalled being hit on the chest by a rifle butt recoil several times while hunting with a locally manufactured rifle.
Chest X-ray did not show significant mediastinal widening. There was no evidence of fracture of the rib or the sternum. A CT brain showed an infarct in the right fronto-parietal region (Fig. 2B). The patient was treated with intravenous labetalol. He subsequently underwent a CT coronary angiogram which was normal followed by Bentall procedure using 25 mm Medtronic Hall valved conduit prosthesis. Bentall procedure is a type of open heart surgery in which an artificial mechanical aortic valve contained within a tubular graft prosthesis is used to replace the aortic valve, aortic root and ascending aorta, with re-implantation of the coronary arteries into the graft. In addition, he had closure of false lumen of the supra-aortic vessels using surgical glue. He recovered well and is doing fine at two year follow up with mild residual left sided weakness with normal daily activities. He is on oral warfarin therapy due to the presence of a mechanical aortic valve with well controlled INR of 2.5.
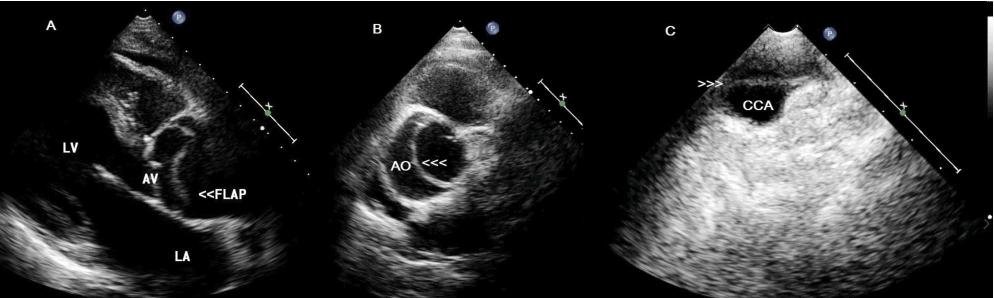
Figure 1: Transthoracic echocardiography showing a dissection flap in the aortic root (A) and (B) extending to right common carotid artery (C) in a patient with Stanford type A aortic dissection. LV=Left ventricle; LA=Left atrium; AV=Aortic valve; AO=Aorta; CCA=Common carotid artery.
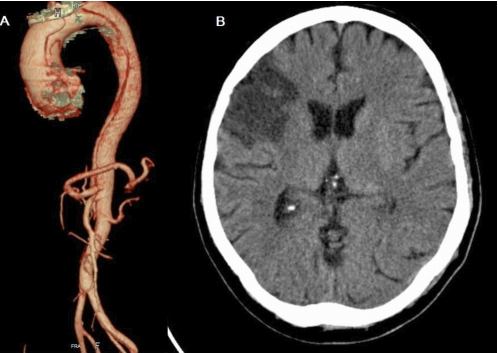
Figure 2: Spiral CT chest image (A) showing aortic root dissection with entry tear just above Sinus of Valsalva and extending into the descending thoracic and abdominal aorta up to left iliac artery. (B) CT brain showing a large infarct in right fronto-parietal region.
Discussion
Various mechanisms have been described for blunt aortic injuries. Many blunt aortic injuries probably involve a combination of forces, including stretching, shearing, torsion, a “water-hammer” effect (which involves simultaneous occlusion of the aorta and a sudden elevation in blood pressure), and the “osseous pinch” effect from entrapment of the aorta between the anterior chest wall and the vertebral column.2,3 Proximal AoD is an extremely rare injury found in the setting of blunt trauma and may be due to trauma causing a tear in the intima or media. It is also postulated that vertical forces of deceleration tend to lead to the rupture or dissection of the ascending aorta, whereas horizontal forces involve the descending aorta.1
In the present case, the rifle butt due to recoil must have struck the chest, of the patient with a force that was vertical to the chest which would have compressed the ascending aorta directly and instantly so that the dissection of the ascending aorta may have occurred due to the mechanisms described earlier. We hypothesize that this patient developed AoD possibly due to rifle butt recoil blunt chest injury, even though spontaneous dissection in a nonhypertensive, non-marfan patient is a possibility. In a study among recreational non-gun shot wound injuries, 43% were caused by gun recoil.4 When a bullet is propelled down the rifle’s barrel, the recoil force normally just pushes the gun back at the shooter; if the recoil is significant it is known to cause lacerations or contusions of the chest, severe bruising or even a broken collar bone.4
Neurologic symptoms are reported in 17-40% of AoD.5,6 Neurologic complications may result from general hypotension, malperfusion, distal thromboembolism, or nerve compression.5 Most occlusions are due to dissection flap prolapsing across a vessel origin (dynamic obstruction) or directly extend into a vessel (static obstruction). Both mechanisms were seen in this patient.
In a recent study by Iguchi et al. among 208 stroke patients presenting within 3 hours of onset, 2 patients (1%) displayed AoD.7 They observed four major findings for stroke with AoD: 1) presentation without pain; 2) with left hemiparesis; 3) negative findings on chest X-ray; and 4) utility of carotid duplex ultrasonography. In the case presented, there was no anterior or interscapular pain typical of AoD, he presented with left hemiplegia and the chest X-ray did not help. Initially, carotid duplex ultrasonography did pick-up a thrombus probably in the false lumen or it could have been an intramural hematoma but dissection was missed. It has been noted that, thrombolysis as an emergency stroke therapy without considering AoD may be life-threatening for these patients.8 In a recent report from the International Registry of Acute Aortic Dissection, D-dimer level has been found to be useful to rule out AoD when used within the first 24 hours after the onset of symptoms.9
Conclusion
We described a patient with left hemiplegia secondary to Stanford type A AoD extending to supra-aortic vessels, which was possibly precipitated by rifle butt recoil chest injury. Furthermore, his AoD was not diagnosed for few weeks due to atypical presentation. This case emphasizes the need for caution in the use of firearms for recreation and to take precautions in preventing such incidents. In addition, this case illustrates need for performing a prompt cardiovascular examination, and maintaining a high index of suspicion in diagnosing AoD among patients with stroke.
Acknowledgements
The authors reported no conflict of interest and funding has been received on this work.
|