|
Introduction
A 40-year old female presented to the Breast Clinic with a painless lump in the right breast for one month with no associated fever, nipple discharge or skin redness. The patient gave a history of a hard, slightly painful lump in the left breast for which she had undergone breast conservation surgery. Review of the records revealed that the patient had an early stage invasive ductal carcinoma. On local inspection, the right breast was normal in size with no nipple retraction and obvious swelling. On palpation; a 5×4 cm soft mobile lump was felt in the upper outer quadrant. It was non-tender and the skin was freely mobile over it. A separate 2×2 cm firm, non-tender, mobile lump was palpated in the upper outer quadrant, below the larger lump. There were no palpable lymph nodes in the axilla. The left breast was asymmetrically small with a large scar as a result of the previous operation. On palpation, no lump could be palpated and there was no axillary lymphadenopathy. The patient was referred to the mammography unit for bilateral mammograms. Selected mammogram (Figs. 1, 2) and ultrasound images (Fig. 3) are given as below.
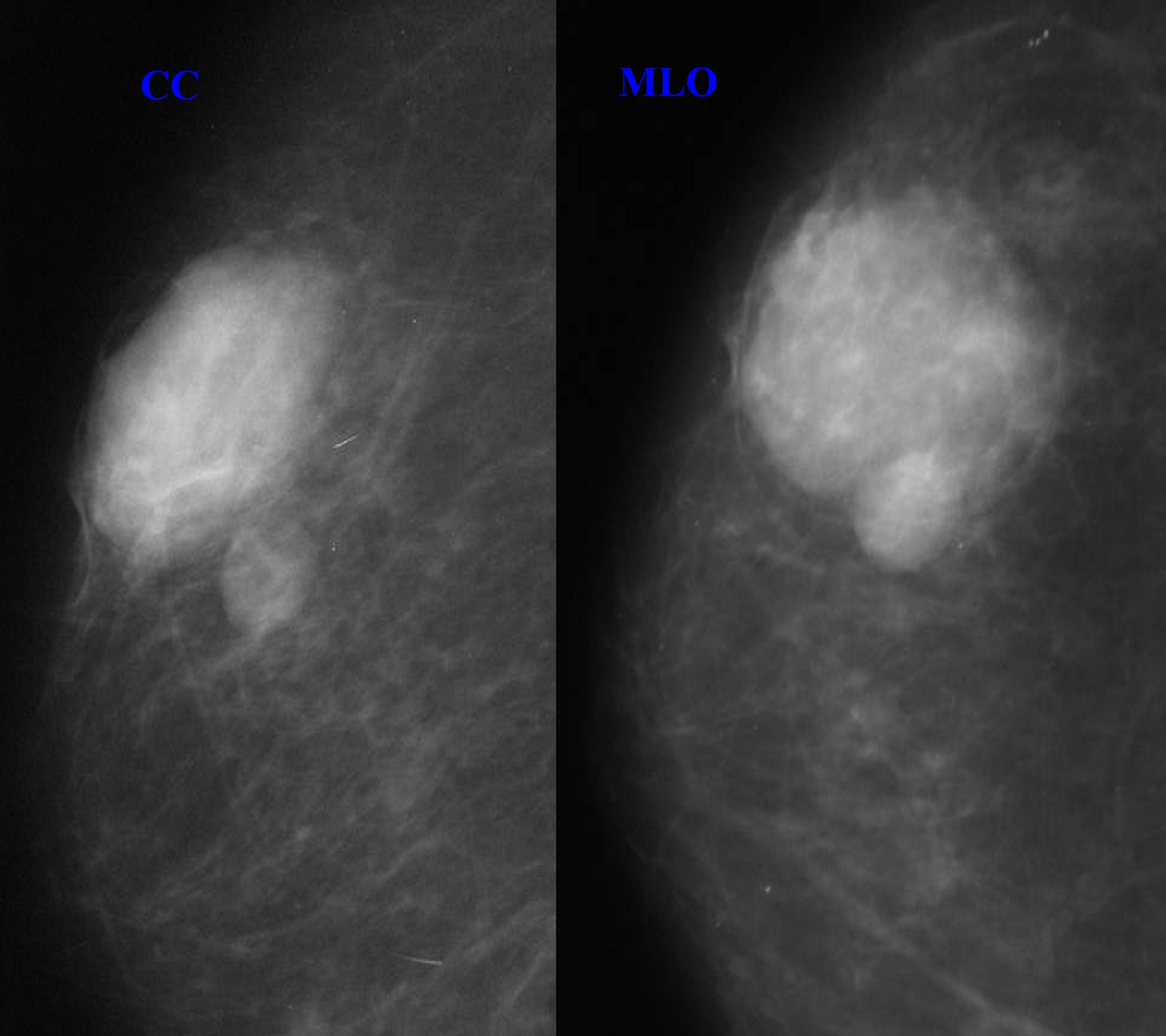
Figure 1: Right mammogram with craniocaudal and mediolateral oblique views show a large mass in the upper outer quadrant with heterogeneous density containing both lucent and dense areas and showing a well-defined margin in part of its circumference. A smaller, well-defined homogeneously iso-dense mass is seen just below this lesion. There are no microcalcifications or architectural distortion.
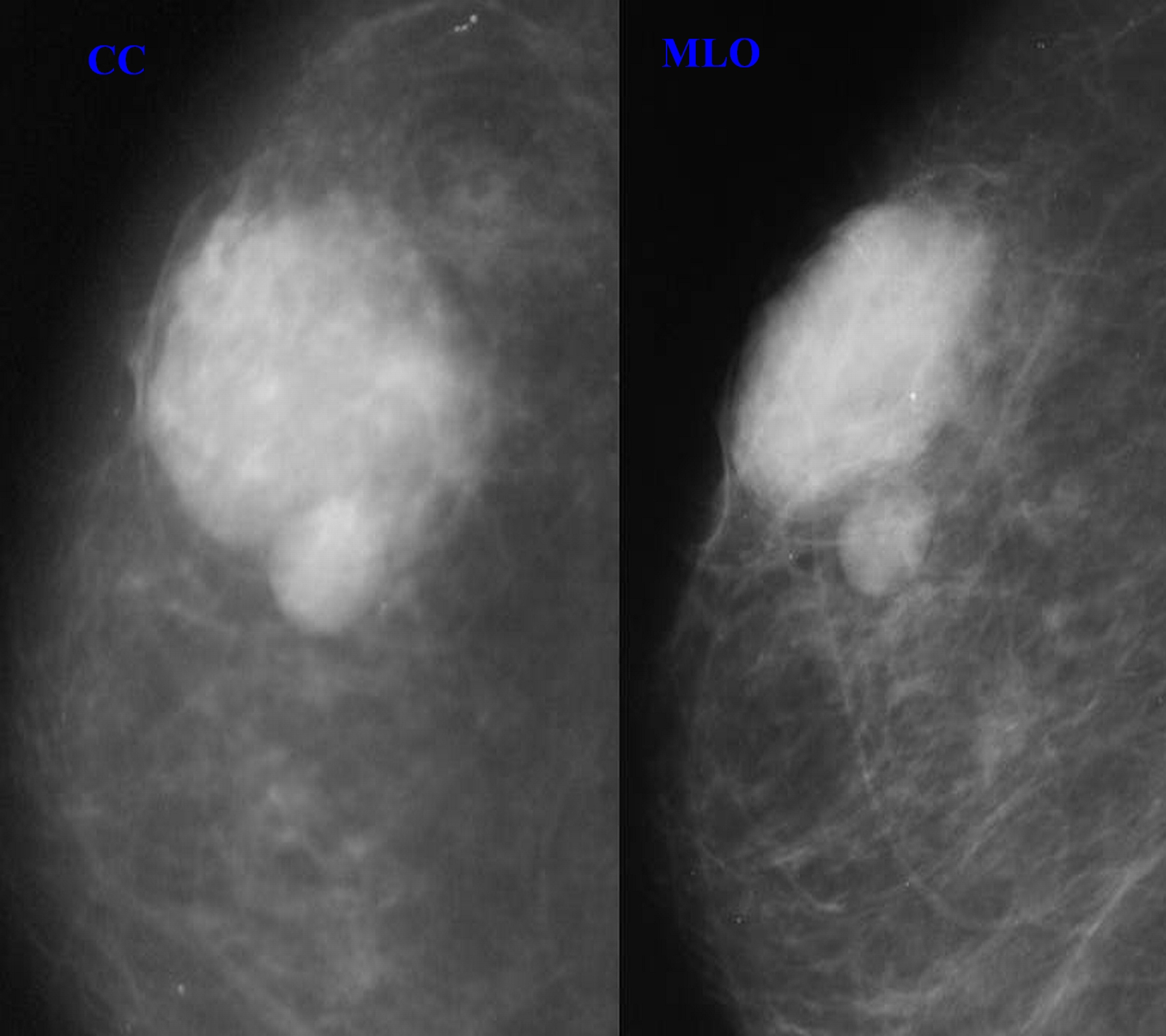
Figure 2: A repeat previous mammogram of the same patient at six months (craniocaudal and mediolateral oblique views). Based on this comparison of the two mammograms more than 6 months apart with no change in the size or density of the lesions, a diagnosis of definite benign lesions could be made.
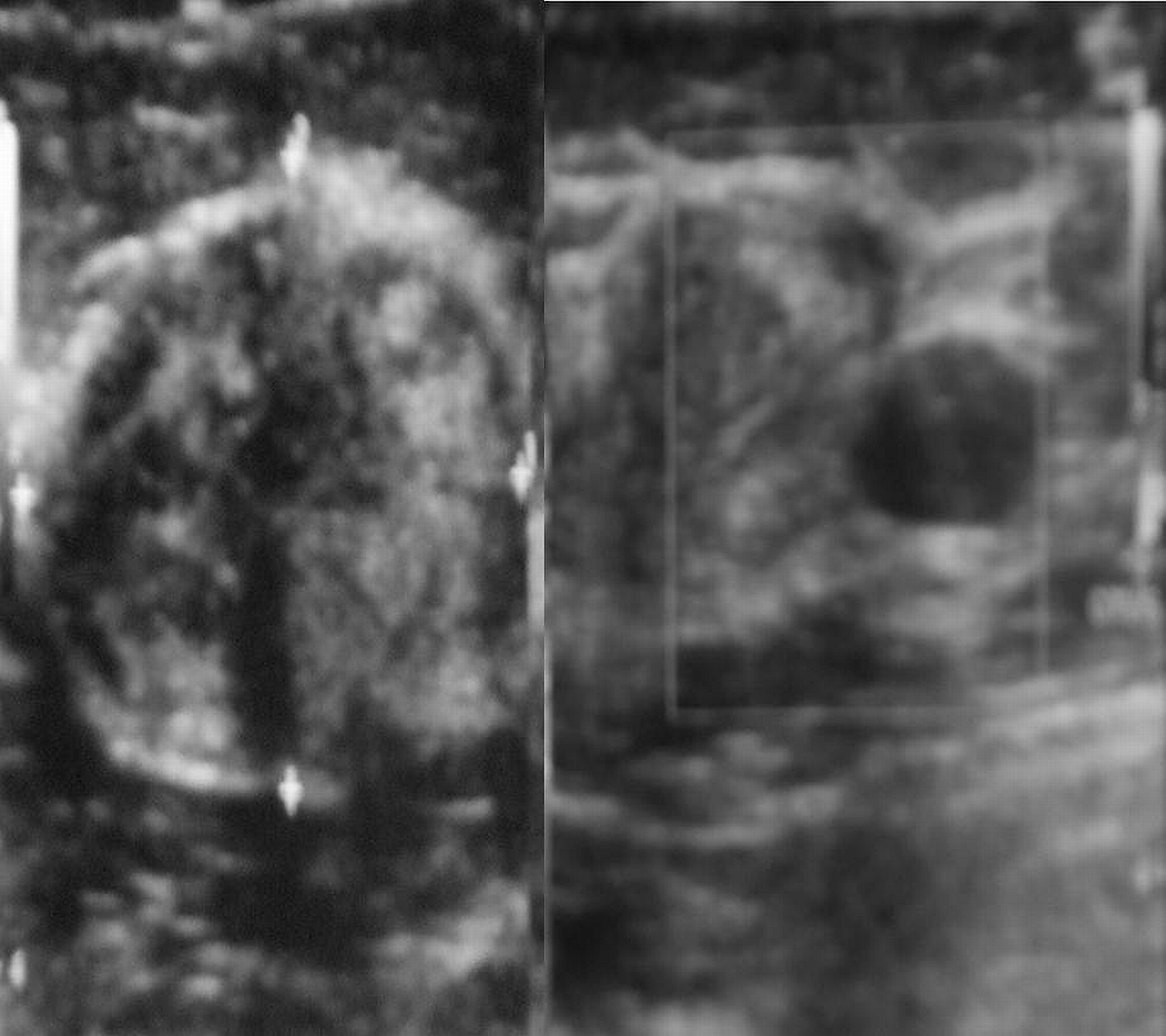
Figure 3: Sagittal and transverse images of the mammographic lesions showing larger lesion (5 × 3.5 cm) to be well defined, transversely oval, heteroechoic with no posterior acoustic shadowing or enhancement, with a well defined capsule around the entire lesion. The smaller lesion (1.5 × 1.5 cm) is roughly round, uniformly hypoechoic with posterior acoustic enhancement. Neither of the two lesions show microcalcifications.
Question
What would be your diagnosis?
Answer
The mammographic and ultrasound appearance of the lesion suggests a diagnosis of breast hamartoma.
Discussion
Hamartoma is a rare benign tumor of the breast. It is known by many synonyms; lipofibroadenoma, fibroadenolipoma or adenolipoma, which is based on the predominant components within the mass.1 The etiology of this disease entity is obscured. It most commonly presents in middle aged females as a painless lump. On examination, more than half of these lesions are soft and non-palpable. Gross pathological examination of a section gives the appearance of a "slice of salami" or "breast within breast."1 The tumor is composed of varying admixture of fibrous, glandular and fatty components. The margin of the tumor is formed by compressed breast parenchyma known as the "pseudocapsule." Histologically; the glandular component forms prominent lobules in matrix containing fat and fibrous stroma. This organization of glandular tissue differentiates hamartoma from fibro adenoma. The mammographic appearance is known as a "piece of cut sausage."2 They are well circumscribed masses with both fat and soft tissue densities, and are surrounded at least partly by a thin radio-opaque line which represents the pseudo capsule.
Based on this classic appearance, a mammographic diagnosis is possible, as was in our patient. The ultrasound appearance is highly variable and it rarely contributes primarily to a differential diagnosis. However, the typical sonographic appearance is that of a well circumscribed solid mass, which is predominantly hypoechoic but has hyper-echogenicity in the form of lines or bands. They have a variable acoustic shadowing. MRI characteristics of hamartoma include; fat density within the mass with smooth well defined hypo-intense rim and heterogenous contrast enhancement. While fine needle aspiration cytology (FNAC) fails to diagnose most of these lesions, mainly due to the scantly material provided by FNAC, as well as the lack of any distinctive architectural or cytological characteristics of hamartoma.1,3 Even a core biopsy may not prove to be useful in the absence of clinical and strong radiological suspicion. The most important clinical and radiological differential diagnoses are fibroadenoma, lipoma, fat necrosis, and galactocele.4
Fibroadenoma appears as a well-circumscribed mass with coarse calcifications of varying morphology; however mammographic appearances can be highly variable. Lipomas are usually not detected on mammography unless they are large, where they are seen as well-defined entirely lucent lesion.5 Fat necrosis has a spectrum of mammographic appearances; however the pathognomonic appearance is that of a lipid cyst which is seen as a well-defined, smooth bordered, round or oval lucent mass with a thin rim which may calcify.6 Typical mammographic appearance of a galactocele is a solitary or multiple masses having density similar to or less than the fibro-glandular parenchyma. The presence of fat-fluid levels within a well-defined mass is pathognomonic.7 Malignancy associated with hamartoma is rare but should be kept in mind. Surgical resection of the mass is the definitive treatment. Follow up of the lesions is recommended as recurrences have been reported in several studies.8
Acknowledgements
The authors reported no conflict of interest and no funding was received for this work.
References
1. Tse GM, Law BK, Ma TK, Chan AB, Pang L-M, Chu WC, et al. Hamartoma of the breast: a clinicopathological review. J Clin Pathol 2002 Dec;55(12):951-954.
2. Paulus DD. Benign diseases of the breast. Radiol Clin North Am 1983 Mar;21(1):27-50.
3. Gogas J, Markopoulos C, Gogas H, Skandalakis P, Kontzoglou K, Stavridou A. Hamartomas of the breast. Am Surg 1994 Jun;60(6):447-450.
4. Pui MH, Movson IJ. Fatty tissue breast lesions. Clin Imaging 2003 May-Jun;27(3):150-155.
5. Lanng C, Eriksen BO, Hoffmann J. Lipoma of the breast: a diagnostic dilemma. Breast 2004 Oct;13(5):408-411.
6. Evers K, Troupin RH. Lipid cyst: classic and atypical appearances. AJR Am J Roentgenol 1991 Aug;157(2):271-273.
7. Gómez A, Mata JM, Donoso L, Rams A. Galactocele: three distinctive radiographic appearances. Radiology 1986 Jan;158(1):43-44.
8. Daya D, Trus T, D’Souza TJ, Minuk T, Yemen B. Hamartoma of the breast, an underrecognized breast lesion. A clinicopathologic and radiographic study of 25 cases. Am J Clin Pathol 1995 Jun;103(6):685-689.
|