| |
Abstract
A 20-year-old female presented to the Pulmonary Medicine Department with complaints of fever, left sided chest pain and progressive dyspnoea of four months duration. Radiological examination revealed a mass lesion with massive pleural effusion and rib erosion. Histopathology showed neoplastic cells with scanty cytoplasm, hyperchromatic nuclei and rosette formation suggestive of Ewing sarcoma. The rarity of this tumor and its unusual presentation prompted this report.
Keywords: Ewing's sarcoma; Pleural effusion; Rib.
Introduction
Ewing's sarcoma (ES) is a malignant neoplasm which accounts for about 1% of all childhood cancers, and primarily involves the bone or soft tissue.1 ES is the second most common malignant bone tumor in the pediatric population.1 The mean age group of ES is 13 with female predilection of approximately 2:1. ES belongs to a family of tumors which comprises of Askin tumor and peripheral primitive neuroectodermal tumor (PPNET).2 The primary bone lesion is usually in the femur, pelvic bones, humerus, fibula, clavicle, or tibia. Rib, scapula and vertebra are the infrequent sites.3,4 We report a case of a teenager who presented with pleural effusion involving the ribs.
Case Report
A previously healthy 20 year-old woman presented to the Pulmonary Medicine Department with complaints of fever, left sided chest pain and progressive breathlessness of four months duration. Her general physical examination was unremarkable except for pallor, while local chest examination revealed fullness, reduced chest expansion, stony dull note and reduced breath sounds on the left side. The rest of the clinical examination was unremarkable. Her routine laboratory analysis was within normal limits, except mild anemia (Ht; 33.6% and Hb; 9.2 mg/dL) and slightly increased erythrocyte sedimentation rate (43 mm/h).
Admission chest X-ray showed homogeneous opacity in the left hemithorax with mediastinal shift, (Fig. 1). Her tuberculin test was negative. Diagnostic thoracentesis revealed a hemorrhagic lymphocytic exudative pleural effusion (total cell count: 30/μl, mainly lymphocytic [60%]); proteins: 3.5g/dl; glucose: 5 mg/dl; LDH: 32 IU/L; adenosine deaminase: 23.6 U/L). The total serum proteins and albumin were 6.2 and 4.5 g/dl respectively. Pleural fluid examination was negative for malignant cells. Computed tomography of the thorax demonstrated large heterogeneous soft tissue mass measuring 19.1×11.5×8.6 cm with gross pleural effusion and collapse of the left lung with cortical destruction and expansion of the costal end of the left 7th rib; suggesting that the lesion was likely to have originated from the rib, (Fig. 2). Finally, a CT guided transthoracic needle biopsy and pleural biopsy with cope needle was done which showed cells with scanty cytoplasm, hyperchromatic nuclei and rosette formation, (Fig. 3). Immunohistochemistry revealed tumor cell cytoplasm positive for CD 99 (a MIC 2 product sensitive for Ewing’s sarcoma but not specific) and negative for CK 7 (marker for synovial sarcoma), (Fig. 4). Based on these findings; the cause of pleural effusion was diagnosed as ES of the 7th rib with extension into the thoracic cavity. With this diagnosis, a chemotherapy regimen with cyclophosphamide, Adriamycin, vincristine and prednisolone (CHOP) was initiated. After two cycles, there was clinical and radiological improvement, (Fig. 5). The patient is currently under regular follow up.

Figure 1: Admission chest X-ray showing homogeneous opacity of left hemithorax with mediastinal shift.

Figure 2: Computed Tomography of the thorax revealing large heterogeneous soft tissue mass with gross pleural effusion and collapse of left lung with cortical destruction and expansion of adjacent 7th rib.
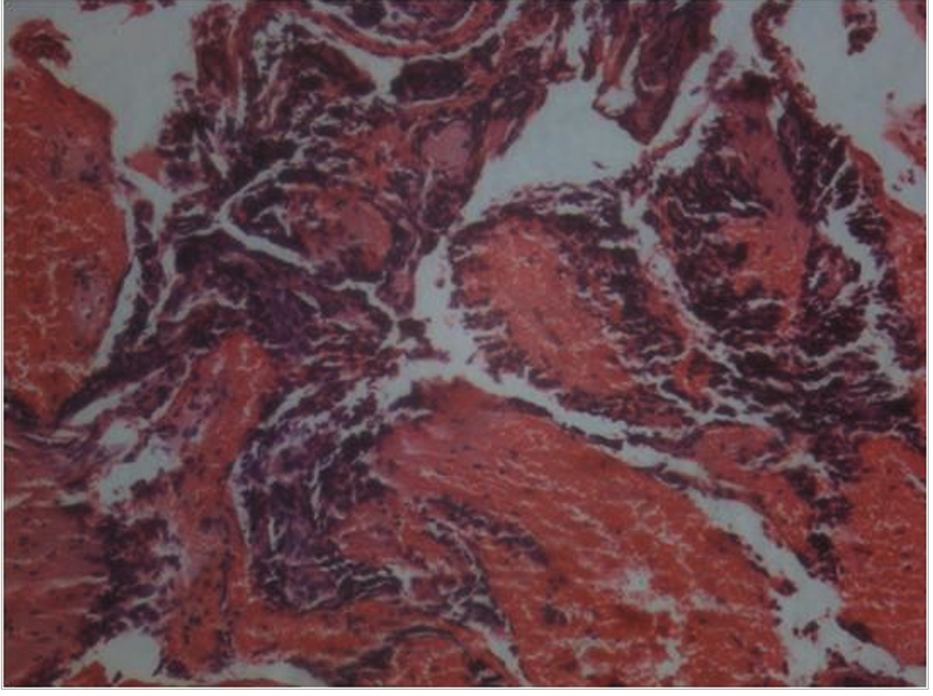
Figure 3: Microphotograph of the biopsy specimen showing tumour cells with scanty cytoplasm and rosette formation (Hematoxylin and Eosin × 125 × digital magnification).
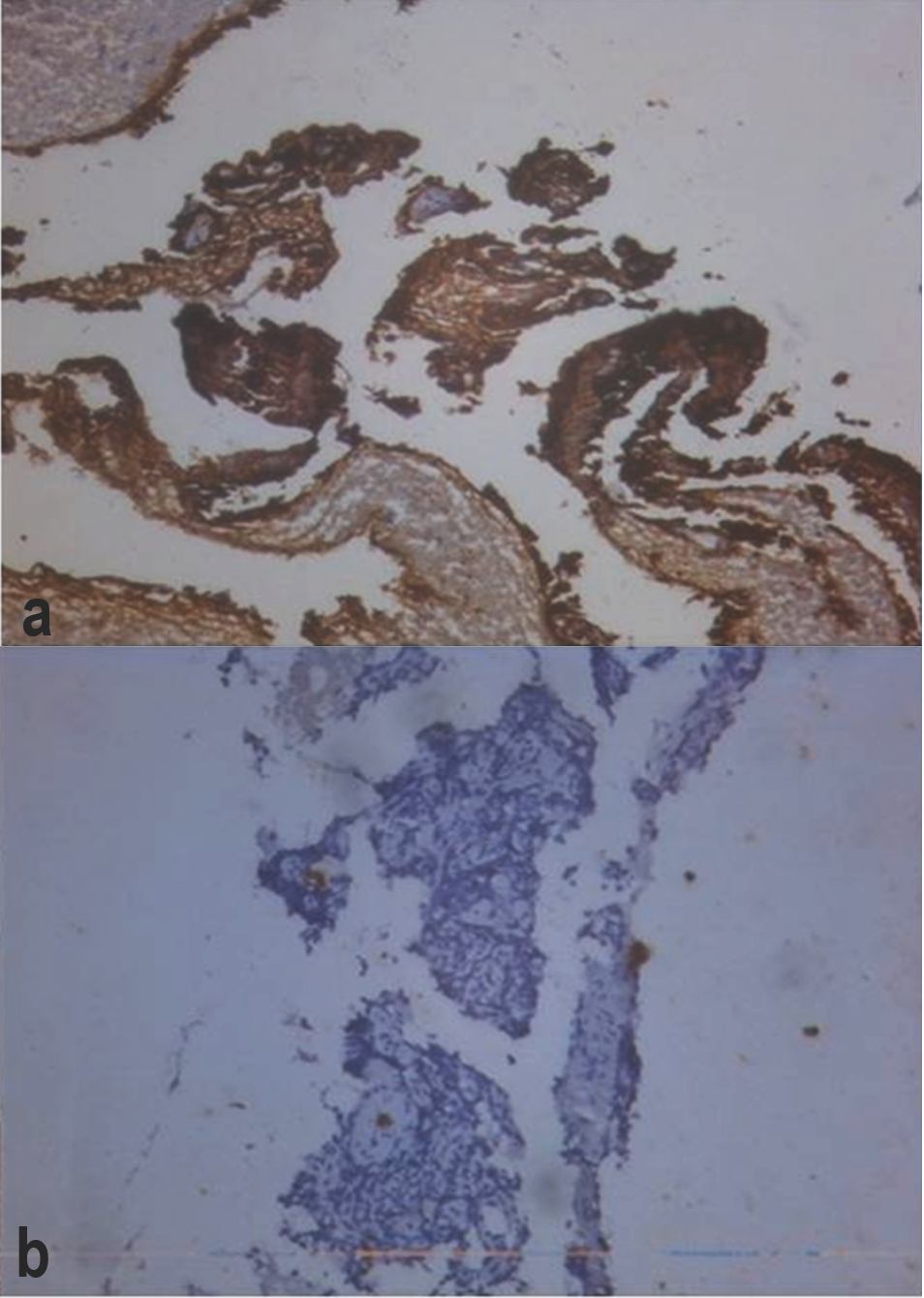
Figure 4: Immunohistochemical analysis demonstrating positive staining for CD 99(a) and negative CK 7(b) in tumor tissue. (Original magnification ×1000; immunoperoxidase stain).
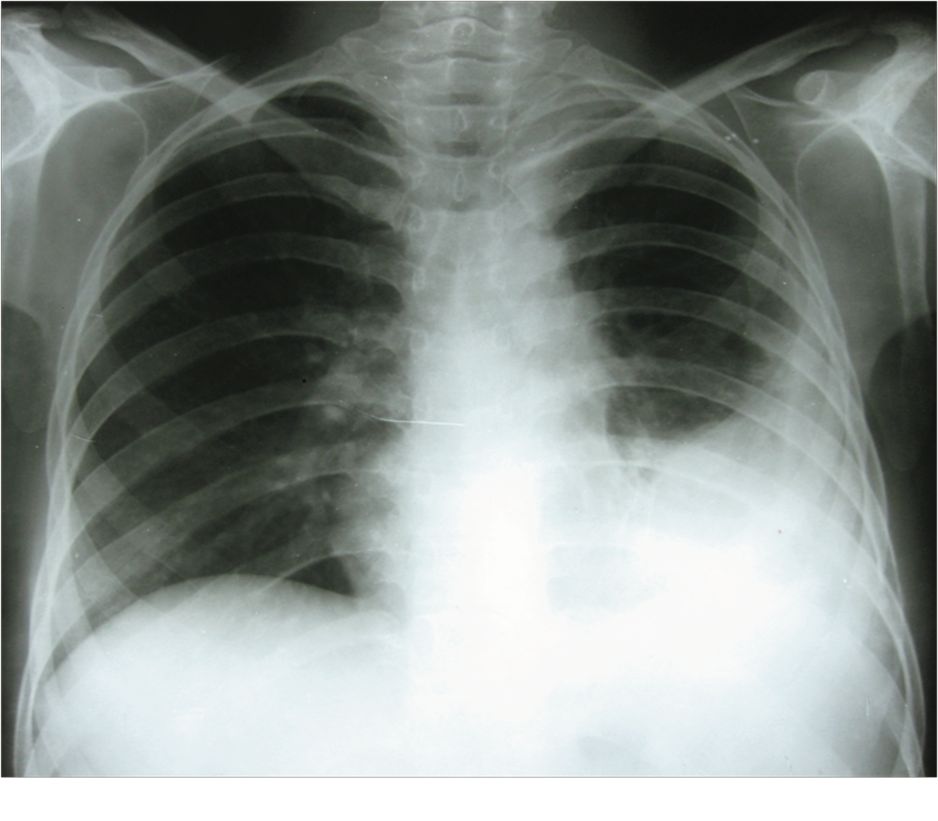
Figure 5: Post two cycles of chemotherapy (CHOP), chest X-ray showing radiological improvement.
Discussion
ES is an uncommon disease, which usually arises from the skeletal bones and most commonly affects children and young adults. A characteristic chromosomal translocation, (11; 22) (q24; q12) can be detected in 90% of cases.5 Patients typically present with painful chest wall mass. The most common systemic symptoms are fever and malaise.6 Presentation of pleural effusion as in our case, is an unusual finding.7,8 ES of the ribs has propensity to spread inwards towards the thoracic cavity and may thus manifest as an extra pleural mass. In the current case report; pleural effusion was secondary to diffuse pleural metastases because pleural biopsy was suggestive of ES. The radiographic appearance of ES of the rib cage is variable. The affected rib is predominantly lytic in most cases, but mixed lytic-sclerotic and even predominantly sclerotic patterns are also encountered.9 Our patient exhibited lytic pattern in the rib. Classically, the affected ribs show increased uptake on bone scintigraphy scanning and the diagnosis is made by biopsy. Optimal treatment is achieved with multi-drug chemotherapy and subsequent resection of the rib and/or radiotherapy. The overall 5- and 10-year survival rates are approximately 50%.
Prognosis is related to tumor volume, tumor resectability, presence of fever, anemia and development of metastases, which occur in 75% of patients; the 5-year survival without metastases approaches 100%, whereas with metastases is less than 30%.6,10 Due to the development of newer chemotherapeutic regimens in recent decades, there has been a remarkable improvement in survival rates.10 Favorable response in our case was due to the timely diagnosis of the disease. The common primary malignancies of ribs are chondrosarcoma and osteosarcomas, but these are uncommon in our patient’s age group.9 However, neuroblastoma and leukemia are common in this group, and their metastases to the rib should be considered in the differential diagnosis. Other conditions that simulate ES are lymphoma, myeloma, osteosarcoma, pleural based masses, eosinophilic granuloma and osteomyelitis.11 The two peculiarities of the present report are; firstly, the patient was older than previous reports of ES with pleural effusion, and secondly, the case highlights the fact that timely diagnosis can increase the survival rate.7,8
Conclusion
In summary, whenever a patient presents with hemorrhagic pleural effusion, especially in tuberculosis endemic countries like India, it is worthwhile to perform histopathological examination before starting the patient on antituberculosis treatment.
Acknowledgements
The authors reported no conflict of interest and no funding was received on this work.
References
1. Iwamoto Y. Diagnosis and treatment of Ewing’s sarcoma. Jpn J Clin Oncol 2007 Feb;37(2):79-89.
2. Sahu K, Pai RR, Khadilkar UN. Fine needle aspiration cytology of the Ewing’s sarcoma family of tumors. Acta Cytol 2000 May-Jun;44(3):332-336.
3. Chan RC, Sutow WW, Lindberg RD, Samuels ML, Murray JA, Johnston DA. Management and results of localized Ewing’s sarcoma. Cancer 1979 Mar;43(3):1001-1006.
4. Chan RC, Sutow WW, Lindberg RD, Samuels ML, Murray JA, Johnston DA. Management and results of localized Ewing’s sarcoma. Cancer 1979 Mar;43(3):1001-1006.
5. Amatruda JF, Tran K, Mantel M, Singer S, Demetri G. Diagnosis in oncology. Askin tumor. J Clin Oncol 1998 May;16(5):1997-1998.
6. Gladish GW, Sabloff BM, Munden RF, Truong MT, Erasmus JJ, Chasen MH. Primary thoracic sarcomas. Radiographics 2002 May-Jun;22(3):621-637.
7. Wolf G, Aigner RM, Schwarz T. Massive pleural effusion with dyspnea in a 17-year-old boy as the first sign of ewing sarcoma. J Pediatr Hematol Oncol 2002 Jun-Jul;24(5):420.
8. Ozge C, Calikoglu M, Cinel L, Apaydin FD, Ozgür ES. Massive pleural effusion in an 18-year-old girl with Ewing sarcoma. Can Respir J 2004 Jul-Aug;11(5):363-365.
9. Franken EA Jr, Smith JA, Smith WL. Tumors of the chest wall in infants and children. Pediatr Radiol 1977 Jul;6(1):13-18.
10. Cotterill SJ, Ahrens S, Paulussen M, Jürgens HF, Voûte PA, Gadner H, et al. Prognostic factors in Ewing’s tumor of bone: analysis of 975 patients from the European Intergroup Cooperative Ewing’s Sarcoma Study Group. J Clin Oncol 2000 Sep;18(17):3108-3114.
11. Kadan-Lottick NS: Cancer and benign tumors, in: Behrman ER, Kliegman R, Jenson HB editors. nelson Text book of Pediatrics. 18th ed. Saunders elsevier, 2007: 2097-2162.
|
|